When you pick up a prescription for a generic drug, you’re probably thinking about saving money. But behind that simple swap - from brand name to generic - lies a complex economic calculation that affects everything from your co-pay to the future of drug innovation. Cost-effectiveness analysis isn’t just accounting. It’s about asking: Is this cheaper drug really giving me the same health outcome? And if it is, why are some generics still priced like luxury brands?
How generics slash costs - and why that matters
Generic drugs aren’t knockoffs. They’re exact copies of brand-name drugs, approved by the FDA after proving they work the same way in the body. But their price? It’s a different story. When the first generic hits the market, the brand-name drug’s price typically drops by 39%. When six or more generic makers enter the race, prices fall more than 95% below the original. That’s not a discount. That’s a revolution. In the U.S., generics made up 90% of all prescriptions filled in 2022. Yet they accounted for just 17% of total drug spending. That’s how powerful this shift is. Over the last decade, generics saved the American healthcare system $1.7 trillion. That’s enough to cover the annual medical bills of every person in Texas and California combined. But here’s the catch: not all generics are created equal in price. Some cost 15 times more than other drugs in the same therapeutic class - even though they treat the exact same condition. A 2022 study looked at the top 1,000 most-prescribed generics and found 45 that were shockingly overpriced. If those 45 were swapped out for cheaper alternatives, total spending would have dropped from $7.5 million to under $900,000. That’s an 88% savings - just by switching to a different generic.What cost-effectiveness analysis actually measures
Cost-effectiveness analysis (CEA) is the tool health systems use to figure out which treatment gives you the most health for your dollar. It doesn’t just look at the sticker price. It measures outcomes too - like how many extra years of healthy life a drug gives you, measured in something called a quality-adjusted life year (QALY). The key number here is the incremental cost-effectiveness ratio, or ICER. It tells you how much extra it costs to gain one more QALY. If Drug A costs $10,000 and gives you 1 QALY, and Drug B costs $12,000 and gives you 1.2 QALYs, the ICER is $10,000 per additional QALY. Health systems set thresholds - often around $50,000 to $150,000 per QALY - to decide what’s worth covering. For generics, the math usually looks great. Most generics have ICERs far below those thresholds. But here’s where things get messy: many cost analyses still use the old brand-name price as the comparison. That’s like measuring how cheap a used car is by comparing it to the original MSRP. It’s misleading. When you compare a generic to the right alternative - another generic in the same class - the savings become even clearer.The hidden problem: high-cost generics
You’d think that once a drug goes generic, prices would race to the bottom. But that’s not always what happens. Some generics stay expensive - sometimes 20 times more than other drugs that do the same job. Why? One reason is formulation. A pill you swallow is cheaper to make than a patch you stick on your skin or a liquid you inject. So if you switch from a generic tablet to a generic patch - even though both treat high blood pressure - the price can jump dramatically. The JAMA study showed that generics with different dosage forms cost 20.2 times more than their simpler counterparts. Another reason? Pharmacy Benefit Managers (PBMs). These middlemen negotiate prices between drugmakers and insurers. But they make money from “spread pricing” - charging insurers one price, paying pharmacies another, and pocketing the difference. If a high-cost generic gives them a bigger spread, they have a financial incentive to keep it on the formulary - even when a cheaper, equally effective option exists. This isn’t theory. It’s happening right now. In 2022, a single generic version of a common cholesterol drug cost $1,200 for a 30-day supply. A different generic, made by another company, did the same job for $12. Both were FDA-approved. Both were chemically identical. The only difference? The PBM’s cut.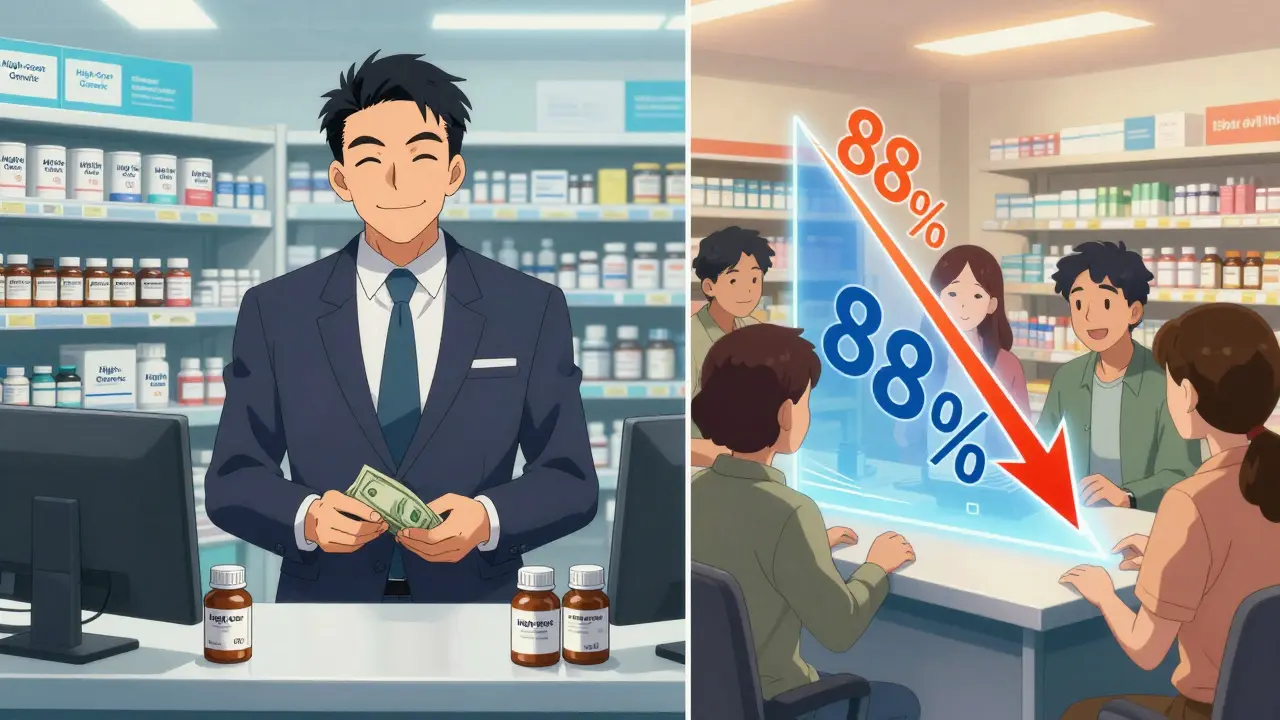
Why most cost analyses get it wrong
Here’s the shocking part: 94% of published cost-effectiveness analyses fail to account for what’s coming next. They don’t model what happens when more generics enter the market. They treat today’s price as if it’s forever. That’s like betting on a stock based on yesterday’s price without checking if the company is about to release a new product. When patent expiration is ignored, CEA can actually work against generics. If the analysis assumes the brand drug will stay expensive, the generic looks like a bargain. But if you know the brand will soon drop to 5% of its original price, the real value isn’t in switching to the generic - it’s in waiting. Experts like Dr. John Garrison warn this creates a dangerous distortion. If health systems base decisions on outdated pricing, they might approve expensive treatments that will soon be replaced by cheaper generics. That wastes money and delays savings. The NIH updated its framework in 2023 to fix this. Now, analysts are told to forecast generic entry and price declines. It’s not easy. You need data on patent timelines, manufacturing capacity, and market demand. But it’s necessary. Without it, cost-effectiveness analysis becomes a snapshot - not a movie.Therapeutic substitution: the underrated savings tool
You don’t always need to switch to the same generic. Sometimes, switching to a different drug in the same class saves even more. Take statins. Atorvastatin (Lipitor) and rosuvastatin (Crestor) are both used to lower cholesterol. After patents expired, generic atorvastatin dropped to pennies per pill. But generic rosuvastatin? It stayed high - sometimes 20 times more expensive. So instead of paying for the pricier generic, doctors can prescribe the cheaper one. Same result. Same safety profile. Lower cost. This is called therapeutic substitution. And according to the same JAMA study, it’s one of the easiest ways to cut drug spending. The study found that when you swap a high-cost generic for a lower-cost alternative in the same class, you can save over 88% - without hurting patient outcomes. But this only works if formularies allow it. Many insurance plans still lock patients into specific brands or generics based on old contracts or PBM deals. Real savings require system-wide changes - not just patient education.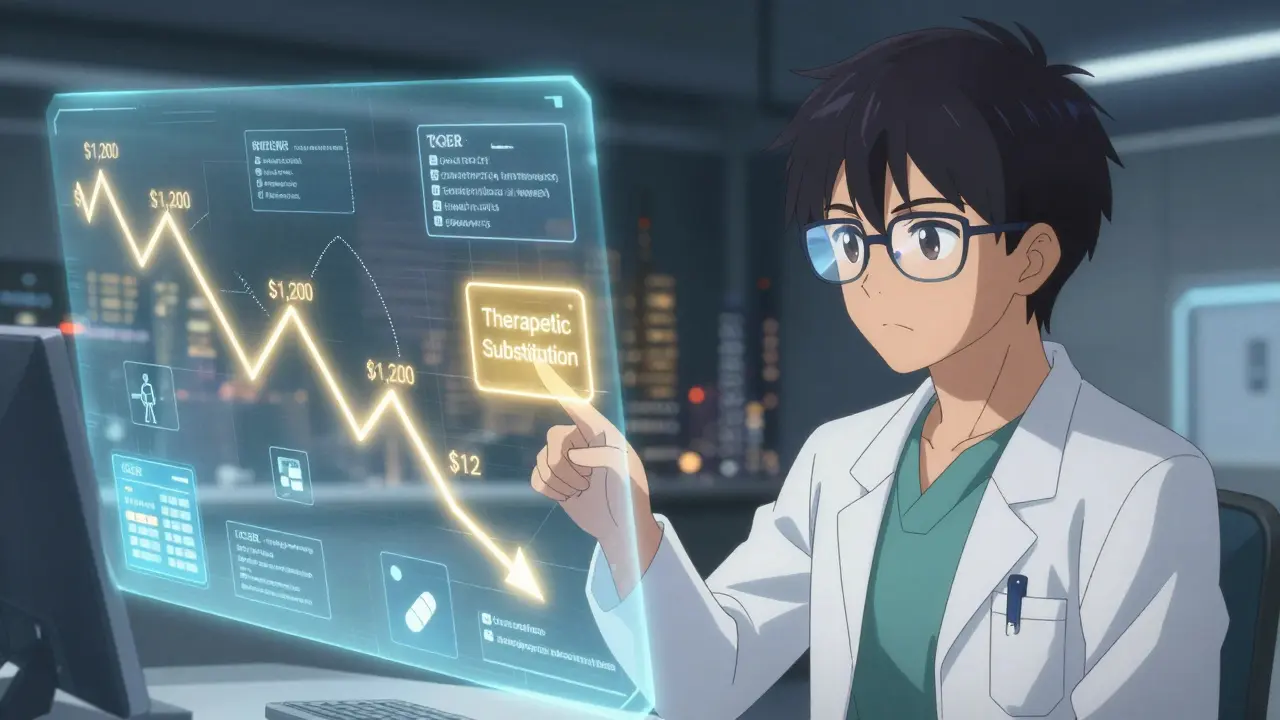
What’s next for generic pricing and cost analysis
Over 300 small-molecule drugs lost patent protection between 2020 and 2025. That means more generics. More competition. More price drops. But also more complexity. The Inflation Reduction Act of 2022 gave Medicare new power to negotiate drug prices. That’s pushing insurers to be smarter about which generics they cover. In Europe, over 90% of health agencies use formal cost-effectiveness analysis to guide coverage. In the U.S., only 35% do - and many still rely on outdated models. The future of CEA isn’t just about today’s prices. It’s about predicting the next wave. Analysts now need to understand patent cliffs, manufacturing trends, and even how drugmakers might delay generic entry with legal tactics. They need to know when a drug will drop to 27% of its AWP (Average Wholesale Price) - the standard used for generics - and when it might spike due to supply shortages. This isn’t just for economists. It’s for pharmacists, doctors, and patients. If you’re on a high-cost generic, ask: Is there a cheaper version that works just as well? If you’re a payer, ask: Are we paying for a PBM’s spread - or a patient’s health?What you can do right now
You don’t need to be an economist to save money on prescriptions. Here’s what works:- Ask your pharmacist: “Is there a lower-cost generic alternative for this drug?”
- Use tools like GoodRx or SingleCare to compare prices across pharmacies.
- Ask your doctor: “Can we switch to a different drug in the same class that’s cheaper?”
- Check your plan’s formulary. If your generic isn’t on the preferred list, request a prior authorization for the cheaper one.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body. Generic drugs go through the same strict manufacturing standards. The only differences are in inactive ingredients - like fillers or dyes - which don’t affect how the drug works.
Why are some generic drugs so expensive?
Some generics stay expensive due to limited competition, complex formulations (like patches or injections), or pricing practices by Pharmacy Benefit Managers (PBMs) who profit from the gap between what insurers pay and what pharmacies are paid. Even when cheaper alternatives exist, PBMs may keep higher-priced generics on formularies if they offer a bigger profit margin.
Can I save money by switching to a different generic?
Absolutely. Two generics for the same condition can have wildly different prices. For example, one generic version of a cholesterol drug might cost $12 for a month’s supply, while another - chemically identical - costs $1,200. Switching to the lower-cost generic can save you over 90%. Always ask your pharmacist or doctor if a cheaper alternative exists.
Does cost-effectiveness analysis favor generics?
When done correctly, yes. Most generics have very low incremental cost-effectiveness ratios (ICERs), meaning they deliver strong health outcomes at minimal cost. But many analyses still use outdated brand prices as comparisons, making generics look better than they might be. The most accurate analyses use current generic prices and forecast future price drops after new competitors enter the market.
How do patent expirations affect generic pricing?
When a drug’s patent expires, generic manufacturers can legally produce and sell it. The first generic typically cuts the price by 39%. With six or more competitors, prices fall over 95% below the original brand price. But if cost-effectiveness analyses ignore this predictable drop, they can mislead decision-makers into approving expensive treatments that will soon become cheap.
What’s the difference between therapeutic substitution and generic substitution?
Generic substitution means switching to a different manufacturer’s version of the same drug. Therapeutic substitution means switching to a different drug in the same class that treats the same condition - like switching from one statin to another. Therapeutic substitution often saves more money because it can bypass high-priced generics entirely and go straight to the cheapest effective option.




Comments (12)