Imagine your kidneys are like fine coffee filters, sifting out waste while keeping precious proteins and blood cells in your body. Now imagine your immune system-designed to protect you-mistakenly turns those filters into a target. That’s glomerulonephritis in a nutshell: an immune attack on the tiny filtering units of your kidneys called glomeruli.
What Exactly Is Glomerulonephritis?
Glomerulonephritis (GN) isn’t one disease. It’s a group of conditions where your immune system goes rogue and damages the glomeruli. These are the microscopic clusters of capillaries in your kidneys that do the heavy lifting of filtering blood. When they get inflamed, they leak protein and blood into your urine, and your kidneys struggle to remove waste. Over time, this can lead to high blood pressure, swelling, and even kidney failure. The damage doesn’t happen overnight. It starts with immune cells or antibodies mistakenly sticking to parts of the glomerular filter-like the basement membrane or the podocytes, the foot-like cells that wrap around the capillaries. Once they latch on, inflammation follows. The body sends in more immune troops, and the glomeruli swell, scar, or collapse.How Your Kidney Filter Works-and How It Breaks
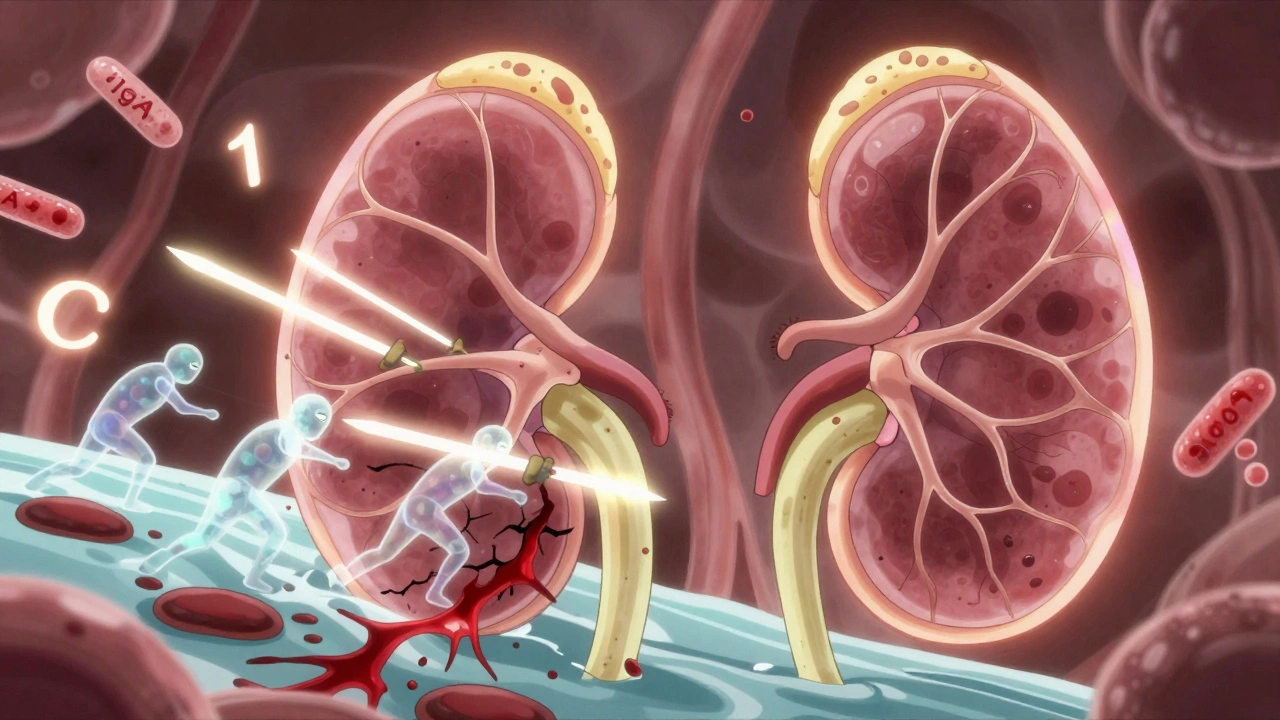
Your glomerulus has three layers: the endothelial cells lining the blood vessel, the basement membrane (a protein mesh), and the podocytes on the outside. Together, they form a selective barrier. Healthy, they let water and waste pass but hold onto proteins like albumin and red blood cells. In GN, this barrier gets breached. In IgA nephropathy, the most common form worldwide, immune complexes made of IgA antibodies build up in the glomeruli. In C3 glomerulonephritis, it’s the complement system-a part of your immune defense-that runs wild, causing C3 protein to pile up at levels 3 to 5 times higher than normal. In lupus nephritis, antibodies from systemic lupus attack the kidneys directly. Podocytes are especially vulnerable. Unlike many cells, they can’t easily repair themselves. Once damaged, they detach, leaving holes in the filter. That’s why proteinuria-large amounts of protein in urine-is a red flag. Levels above 3.5 grams per day mean you’re in nephrotic syndrome territory: swelling in the legs, high cholesterol, and low blood protein.Two Main Faces of Glomerulonephritis
GN doesn’t present the same way for everyone. It usually shows up as one of two syndromes:- Nephritic syndrome: Blood in the urine (hematuria), high blood pressure, reduced kidney function, and swelling. Creatinine levels often rise to 1.5-3.0 mg/dL. This is common in post-streptococcal GN, which hits kids hard but usually resolves in 6-8 weeks.
- Nephrotic syndrome: Massive protein loss (>3.5g/day), low blood protein (<3.0 g/dL), high cholesterol (LDL often >160 mg/dL), and severe edema. This is typical in IgA nephropathy and C3G when they progress.
Common Types and Who Gets Them
Not all GN is the same. Here’s what you’re most likely to encounter:- IgA nephropathy: The #1 cause of primary GN globally. In North America, it affects about 2.5 per 100,000 people a year. In East Asia, it’s twice as common. About 20-40% of patients develop kidney failure over 20 years.
- C3 glomerulonephritis (C3G): A rare form, affecting 1-2 per million people. It’s driven by autoantibodies like C3 nephritic factor (C3NeF), which hijack the complement system. About 60-70% of cases involve these rogue antibodies.
- Lupus nephritis: Hits 50-60% of people with systemic lupus. With modern treatment, 70-80% avoid kidney failure after 10 years.
- Post-streptococcal GN: Usually follows a strep throat or skin infection. Almost all kids recover fully. Adults? Less so.
- Immune Complex-Mediated MPGN: Involves immune complexes stuck in the glomeruli. Biopsies show dense deposits in 95% of cases.
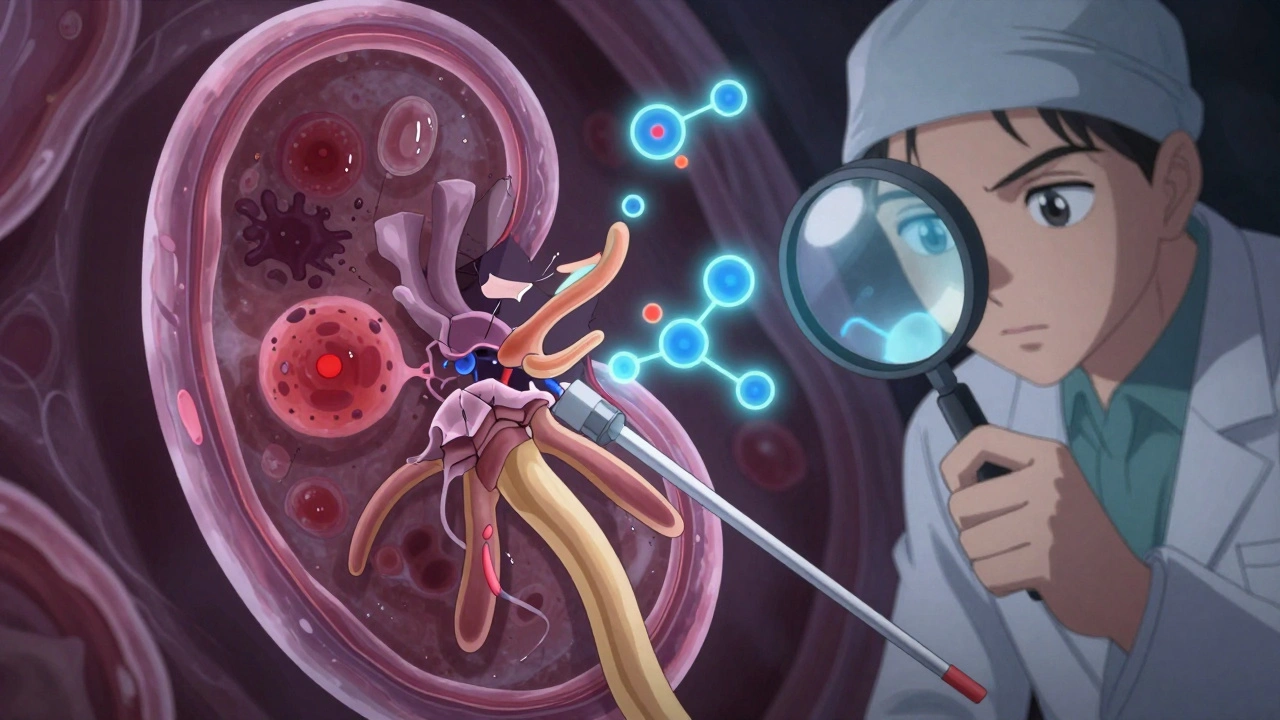
Diagnosis: Why a Kidney Biopsy Is Non-Negotiable
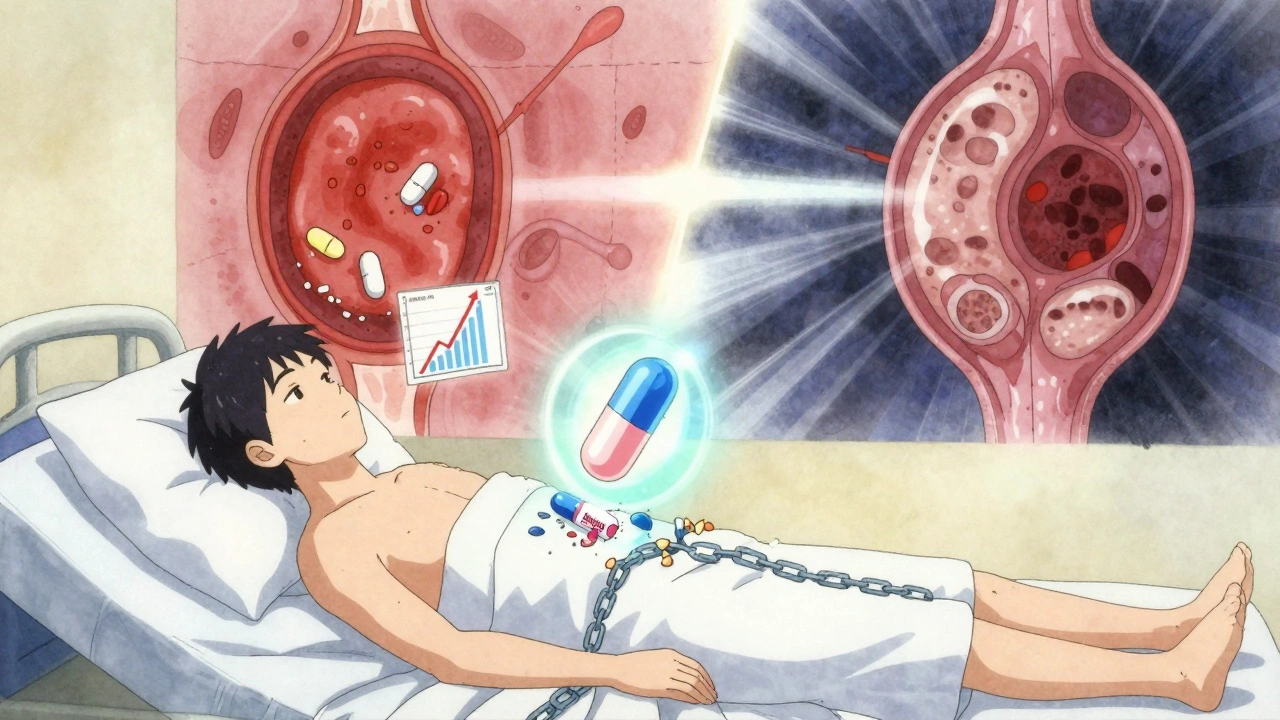
You can’t diagnose GN with a blood test alone. Urine tests might show blood or protein. Blood tests might show high creatinine or low albumin. But only a kidney biopsy can tell you which type you have. The biopsy involves inserting a thin needle into the kidney to pull out a tiny tissue sample. It’s safe in experienced hands, but carries a 3-5% risk of bleeding. Recovery takes a few days of rest. Interpreting the biopsy? That’s where it gets hard. Nephropathologists need 5-7 years of training to spot the difference between C3G and IC-MPGN under the microscope. One misread, and you get the wrong treatment.Treatment: Steroids, Side Effects, and New Hope
For decades, the go-to treatment has been corticosteroids like prednisone. About 60-80% of patients respond at first. But here’s the catch: 30-50% of them relapse, and side effects are brutal.- Weight gain (72% of patients)
- Bone loss leading to fractures (28%)
- Increased infections (35%)
What Patients Are Really Saying
On Reddit’s r/kidneydisease, a common theme: “It took me 4.2 months to get a diagnosis. I saw three doctors.” Patients report:- 78% struggle with swelling they can’t control
- 63% fear steroid side effects more than the disease
- 51% live with constant anxiety about kidney failure
The Future: Personalized Medicine Is Coming
Researchers are moving beyond “one-size-fits-all” treatment. Dr. Richard Lafayette from Stanford predicts that within five years, genetic and protein profiles will guide therapy. Instead of guessing with steroids, doctors will test for C3NeF, IgA patterns, or complement gene mutations-and pick the right drug from the start. New classification systems now combine biopsy results with molecular markers. One study showed 85% accuracy in predicting treatment response-up from 65% with biopsy alone. But here’s the dark side: access. In low-income countries, patients have 70% less access to advanced diagnostics and 90% less access to new drugs. Glomerulonephritis isn’t just a medical problem-it’s a global equity issue.What You Can Do
If you’ve been told you have protein in your urine or blood in your urine:- Don’t wait. See a nephrologist ASAP.
- Track your blood pressure daily.
- Reduce salt intake-this helps control swelling and blood pressure.
- Ask about a biopsy if your doctor hasn’t mentioned it.
- Join a patient group. You’re not alone.
Why This Matters
Glomerulonephritis causes 10-15% of new kidney failure cases in the U.S.-that’s 12,000 to 18,000 people a year starting dialysis because their immune system turned on their kidneys. The global market for GN treatments is set to hit $4.7 billion by 2028. That’s not just business. It’s proof that science is finally catching up to the complexity of this disease. This isn’t just about kidneys. It’s about how your immune system, meant to protect you, can become your greatest threat. And now, for the first time, we’re learning how to stop it-without wrecking the rest of your body.Can glomerulonephritis be cured?
Some forms of glomerulonephritis, like post-streptococcal GN in children, can resolve completely. Others, like IgA nephropathy or C3G, are chronic but manageable. With early diagnosis and the right treatment, many patients can stop progression and live normal lives without dialysis. A cure isn’t guaranteed, but remission is possible.
Is glomerulonephritis hereditary?
Most cases aren’t inherited. But certain rare forms, like Alport syndrome or some types of C3G, have genetic links. If multiple family members have kidney disease, especially with hearing loss or eye problems, genetic testing may be recommended.
Can I still exercise with glomerulonephritis?
Yes-moderate exercise is encouraged unless you have severe high blood pressure or advanced kidney damage. Walking, swimming, and cycling help control blood pressure and reduce fatigue. Avoid heavy weightlifting or contact sports if you’re on immunosuppressants or have low platelets.
What foods should I avoid with glomerulonephritis?
Limit sodium (salt) to reduce swelling and blood pressure. Avoid processed foods, canned soups, and fast food. If your kidneys are significantly damaged, you may also need to limit potassium and phosphorus. A renal dietitian can help tailor this to your needs.
How long does it take to diagnose glomerulonephritis?
On average, patients wait 4.2 months from symptom onset to diagnosis. Many see three or more doctors before getting a biopsy. Early signs like blood in urine, foamy urine, or unexplained fatigue should prompt a referral to a nephrologist. Don’t wait for swelling-it often appears late.
Are there alternatives to steroids for treating glomerulonephritis?
Yes. For IgA nephropathy, SGLT2 inhibitors like dapagliflozin are now recommended alongside blood pressure meds. For C3G, drugs like iptacopan and eculizumab target the complement system directly. Rituximab is used for some immune complex types. These options avoid the worst side effects of long-term steroids.
Can glomerulonephritis come back after a kidney transplant?
Yes, especially IgA nephropathy and C3G. Up to 50% of IgA patients see recurrence in the new kidney, sometimes within months. C3G can also return. Doctors monitor closely in the first year and may start preventive treatment if early signs appear.

Comments (14)