Every time you pick up a prescription for a generic drug, you’re holding a product that’s been through one of the most tightly controlled manufacturing processes in the world. It’s not just a cheaper copy. It’s a scientifically engineered duplicate - down to the last molecule - that works exactly like the brand-name version. But how do companies make sure it’s truly the same? And what happens behind the scenes in a factory that turns powders and chemicals into pills you swallow every day?
The Legal Backbone: The Hatch-Waxman Act and ANDA
The whole system started with a law passed in 1984: the Hatch-Waxman Act. Before this, generic drug makers had to run full clinical trials to prove their drugs worked - just like the original brand did. That cost billions and took over a decade. The law changed that. It created the Abbreviated New Drug Application, or ANDA. This meant generic companies didn’t need to repeat the safety and effectiveness studies already done by the brand-name maker. Instead, they just had to prove their version was bioequivalent. Bioequivalence means the generic drug releases the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA requires that the generic’s absorption - measured by Cmax and AUC - falls within 80% to 125% of the original. That’s not a wide margin. It’s tight enough to ensure that even for drugs like blood thinners or epilepsy meds, where tiny differences can matter, the generic will work just as well. The ANDA process isn’t quick. It takes 3 to 4 years on average and costs between $5 million and $10 million per drug. Compare that to the $2.6 billion and 10-15 years it takes to bring a brand-new drug to market. That’s why generics make up 90% of all prescriptions in the U.S. - they’re affordable without sacrificing safety.Step 1: Reverse Engineering the Brand-Name Drug
Before a single pill is made, the generic manufacturer has to figure out exactly what’s in the original drug. This isn’t just reading the label. It’s deep science. They take the brand-name product apart - chemically analyze every component - to identify the active pharmaceutical ingredient (API) and all the inactive ingredients, called excipients. These include fillers like lactose, binders like starch, and coatings that control how fast the pill dissolves. This stage is called characterizing the Reference Listed Drug (RLD). It’s critical because even small differences in excipients can change how the drug behaves in your body. For example, a change in the particle size of lactose can alter tablet hardness or how quickly the drug dissolves. One pharmaceutical engineer on Reddit with over a decade of experience said, “The biggest headache in generic manufacturing is excipient variability.” A supplier switches to a slightly different grade of magnesium stearate? Suddenly, your tablets don’t hold shape right. That’s why manufacturers test dozens of batches from multiple suppliers before settling on one.Step 2: Designing the Formula - Quality by Design
Once they know what’s in the original, they build their own version using a framework called Quality by Design (QbD). This isn’t just mixing ingredients. It’s a scientific approach that maps out every variable that could affect the final product. They identify three key things:- Critical Quality Attributes (CQAs): What properties must the pill have? Dissolution rate, tablet hardness, purity, uniformity.
- Critical Material Attributes (CMAs): What properties of the raw materials matter? Particle size, moisture content, flowability of powders.
- Critical Process Parameters (CPPs): What steps in manufacturing must be tightly controlled? Mixing time, compression pressure, drying temperature.
Step 3: The Manufacturing Line - Seven Stages, Zero Room for Error
Now it’s time to make the drug. The process follows seven precise steps, all happening in cleanrooms that meet ISO Class 5-8 standards. Temperature is kept at 20-25°C, humidity at 45-65%. Dust and airborne particles are filtered out. Why? Because even a speck of dirt can contaminate a batch.- Formulation: The API and excipients are weighed with extreme precision - often to the milligram. A mistake here means every pill in the batch is wrong.
- Mixing and Granulation: Powders are blended until uniform. Then they’re turned into granules - small clumps - so they flow better during pressing. This step alone can take hours, with multiple rounds of testing to ensure even distribution.
- Drying: Granules are dried to remove moisture. Too much water? The pills degrade. Too little? They crumble. Temperature and airflow are monitored continuously.
- Compression and Encapsulation: For tablets, granules are pressed into shape using high-pressure machines. For capsules, powder is filled into gelatin shells. Tablet weight must be within ±5% for pills under 130mg, or ±7.5% for those between 130-324mg. The FDA checks this on every batch.
- Coating: Tablets get a thin outer layer. This can mask taste, protect the drug from stomach acid, or control release time. Some coatings are designed to dissolve only in the intestine - not the stomach.
- Quality Control: This isn’t one test at the end. It happens at every stage. Each batch is tested for identity, strength, purity, and dissolution. Dissolution testing simulates how the drug breaks down in the body. If it doesn’t release 85% of the active ingredient within 30 minutes (as required), the batch is rejected.
- Packaging and Labeling: Pills go into blister packs or bottles. Labels must match the brand-name drug exactly - same dosage, same warnings, same instructions. But here’s the catch: the pill’s color or shape can be different. U.S. trademark law forbids generics from looking identical to the brand. So a blue oval pill might become a white round one. But the active ingredient? Still the same.
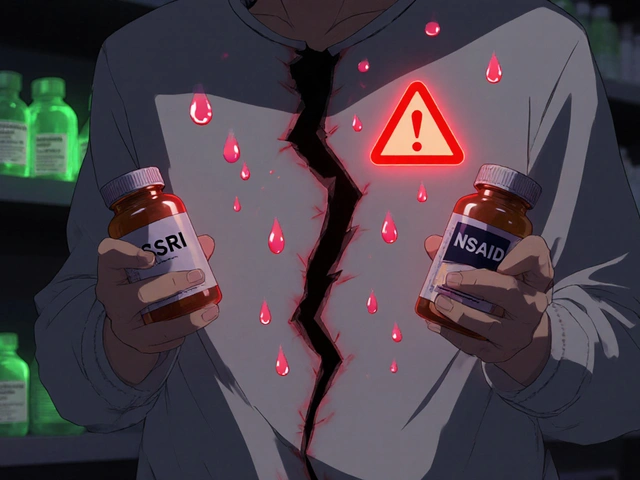
Regulatory Oversight: CGMP and the FDA’s Watchful Eye
Every step must follow Current Good Manufacturing Practices (CGMP). These aren’t suggestions - they’re legally binding rules. Facilities are inspected regularly. In 2023, the FDA found the top three issues in generic drug plants:- 37% failed to properly investigate out-of-specification test results
- 29% didn’t fully validate their manufacturing processes
- 24% had weak oversight from their quality control teams




Comments (15)