When a patient walks into a clinic with a prescription for a brand-name drug, the provider has a choice: hand it over as-is, or ask if they’d be open to a cheaper, equally effective generic version. It’s not just about saving money-it’s about making sure the patient actually takes the medicine. Too often, patients stop taking their meds because they can’t afford them. And when that happens, their condition gets worse, hospitals fill up, and costs spiral. The solution isn’t complicated: generic medications work just as well, and providers are in the best position to make that clear.
Why Generic Drugs Are Just as Safe and Effective
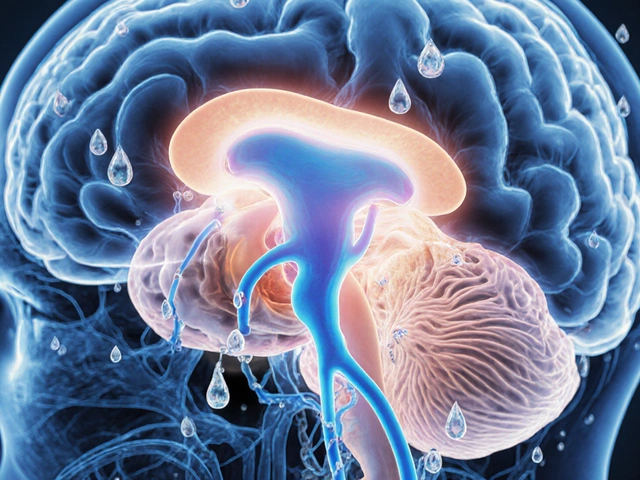
Many patients believe generics are inferior. They think, "If it looks different, it must be weaker." But that’s not how the science works. The FDA requires every generic drug to prove it delivers the same active ingredient, in the same strength, and the same way into the body as the brand-name version. That’s called bioequivalence. The difference in how much medicine enters the bloodstream between a generic and brand drug must be within 80% to 125%. That’s not a guess-it’s a strict, scientifically proven standard. Thousands of studies confirm this. A 2019 report from the Association for Accessible Medicines analyzed over 1.4 billion prescriptions and found no difference in effectiveness between generics and brand-name drugs for conditions like high blood pressure, diabetes, and depression. The only real differences? The color, shape, or filler ingredients. These don’t affect how the drug works. But they do cause confusion. Patients see a new pill and think, "This isn’t the same." That’s why providers need to explain it before the switch happens-not after the patient complains.The Cost Gap Is Huge-and It Matters
Let’s talk numbers. In 2022, generics made up 90% of all prescriptions filled in the U.S. But they accounted for only 23% of total drug spending. Why? Because they’re cheaper. Once a brand-name drug’s patent expires, multiple companies can make the generic. Competition drives prices down. Within a year, generics often cost just 15% of the original brand price. The real kicker? Copayments. For brand-name drugs, 61% of copays were over $20. For generics? 90% were under $20. That’s not a small difference. It’s the line between taking your medicine and skipping doses. The same 2019 study showed that patients are 266% more likely to abandon a brand-name prescription than a generic one-purely because of cost. That’s not laziness. That’s survival. If a patient has to choose between insulin and groceries, they’ll skip the insulin. Providers who don’t talk about cost aren’t just missing a chance-they’re risking harm.What Providers Should Say (and When)
Most doctors and pharmacists know generics are safe. But they don’t always say it. A patient might hear, "We’re switching you to a generic," and assume it’s a cost-cutting move, not a care move. That’s where communication fails. Here’s what works:- "This generic has the same active ingredient as your old pill. It’s been tested to work exactly the same way."
- "Your copay will drop from $45 to $12. That’s the difference between buying your medicine and skipping it."
- "It might look different-different color or shape-but that’s just because the company that makes it uses different fillers. The medicine inside is the same."
- "If you’ve had trouble with this drug before, we can talk about that. But if it’s just because it looks different, I can assure you it’s safe."

When Not to Switch
Not every drug should be swapped. Some medications have a narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is very small. Think warfarin, levothyroxine, or certain seizure drugs. For these, switching between brands or generics can sometimes cause issues. But here’s the truth: the problem isn’t the generic. It’s switching too often. Patients on levothyroxine, for example, might get switched to a different generic every few months. Each time, the inactive ingredients change. Even though the active ingredient is the same, some patients report feeling off. That’s not because generics are unsafe-it’s because their body got used to one formulation. The American Academy of Family Physicians rightly opposes mandatory substitution for these drugs. But they also say providers should work with patients to find one stable generic and stick with it. Consistency matters more than the brand name.Barriers Providers Face-and How to Overcome Them
Time is the biggest obstacle. Most primary care visits last 13 to 16 minutes. Talking about meds feels like a luxury. But here’s the flip side: if a patient stops taking their blood pressure pill because they can’t afford it, you’ll see them back in three months with a stroke. That visit takes hours. The cost? Thousands of dollars. The risk? Permanent damage. Another barrier? Insurance rules. Some plans require prior authorization for brand-name drugs-even when a generic exists. That delays treatment by an average of 2.3 days. The American Academy of Family Physicians has pushed to eliminate prior authorizations for generics. Providers can help by checking their EHR systems for cost alerts. Many now flag when a brand drug costs 10x more than a generic. Use those alerts. Speak up. And don’t forget the pharmacy. Pharmacists are often the first to hear patient concerns. If a patient says, "Why does this pill look different?"-the pharmacist should be trained to answer before the patient leaves. A simple, "This is the same medicine, just made by a different company. Your copay is lower because of it," can prevent abandonment.
The Bigger Picture: Why This Is Patient Advocacy
Advocacy isn’t just about fighting for better policies or protesting drug prices. It’s also about what happens in the exam room. When a provider chooses a generic-not because it’s cheaper for the system, but because it’s better for the patient’s life-that’s advocacy. It’s saying, "I see you. I know this cost matters. And I’m not just writing a prescription-I’m helping you stay healthy." The American College of Physicians says doctors should prescribe generics whenever possible. That’s not a suggestion. It’s a standard of care. And the data backs it up: higher generic use = better adherence = fewer hospitalizations = lower costs. This isn’t about pushing pills. It’s about removing barriers to health. A patient who can afford their medicine is more likely to take it. A patient who understands it’s safe is more likely to trust their provider. And a provider who speaks up? That’s the one patients remember.What’s Next for Generic Medications?
There’s a new challenge: some generic drugs are getting more expensive. In 2023, the American Society of Health-System Pharmacists warned that price spikes for certain essential generics-like insulin, antibiotics, and heart medications-are creating new access problems. This isn’t the norm, but it’s happening. That means providers need to stay alert. Just because a drug is generic doesn’t mean it’s always affordable. Check prices. Ask patients if they’re struggling. Adjust when needed. The future? More tools. Electronic health records are starting to show real-time cost comparisons at the point of prescribing. Some systems even suggest the lowest-cost generic available. Providers who use these tools will save patients money-and time.Final Thought: It’s Not Just a Prescription. It’s a Promise.
When you write a prescription, you’re making a promise: "This will help you." But if the patient can’t afford it, that promise breaks. Choosing a generic isn’t a shortcut. It’s a commitment to real care. It’s saying, "I won’t just treat your condition-I’ll make sure you can live with it." Talk to your patients. Explain the science. Show them the numbers. And don’t assume they know generics are safe. Most don’t. But they trust you. Use that trust. It’s the most powerful tool you have.Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generics to prove they deliver the same active ingredient in the same amount and at the same rate as the brand-name drug. This is called bioequivalence, and it’s tested using strict scientific standards. Studies analyzing over a billion prescriptions have found no difference in effectiveness between generics and brand-name drugs for conditions like high blood pressure, diabetes, and depression.
Why do generic pills look different from brand-name ones?
Generics can look different because they use different inactive ingredients-like dyes, fillers, or coatings-that don’t affect how the medicine works. These differences are allowed under FDA rules, as long as the active ingredient is identical. Patients often mistake the change in appearance for a change in strength, which is why providers should explain this before switching.
When should a provider avoid switching to a generic drug?
For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or certain seizure medications-small changes in blood levels can matter. While generics for these drugs are still safe, frequent switching between different generic versions can sometimes cause instability. The best approach is to pick one generic and stick with it, rather than switching back and forth. Providers should monitor patients closely in these cases.
Do insurance plans encourage the use of generics?
Yes. Most insurance plans and pharmacy benefit managers structure copays so generics cost significantly less-often under $20-while brand-name drugs can cost $40, $60, or more. Some plans even require patients to try a generic first before covering the brand. This isn’t just about saving money for insurers-it’s about helping patients afford their meds.
What if a patient refuses a generic because they don’t trust it?
Don’t force it. Instead, ask why they’re hesitant. Often, it’s based on myths or past experiences. Share facts: "The FDA tests every generic before it’s sold. It has the same active ingredient and works the same way." Mention that 90% of prescriptions filled in the U.S. are generics-and most patients take them without issue. If they still resist, consider whether the brand is truly necessary, or if there’s another generic option they might feel more comfortable with.
Can generic drugs become too expensive?
Yes. While most generics are cheap, some essential ones-like certain antibiotics, insulin, or heart medications-have seen sharp price increases in recent years due to supply issues or lack of competition. Providers should check current prices and be ready to switch to alternatives if a generic becomes unaffordable. The goal is affordability, not just the label "generic."


Comments (10)