Why Patients Still Doubt Generic Medications
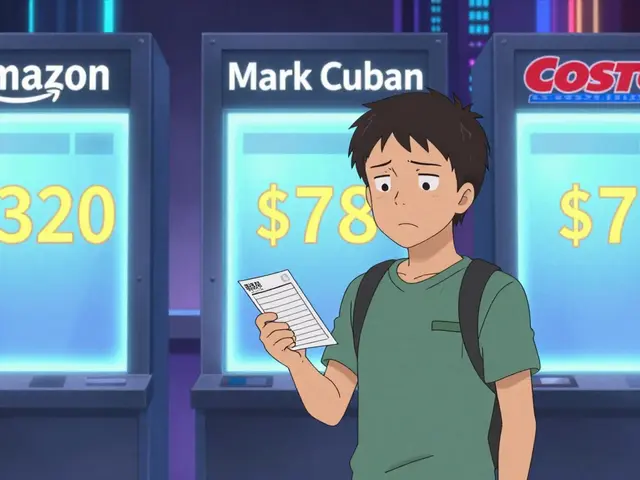
Over 90% of prescriptions filled in the U.S. are for generic drugs. They cost 80% less than brand-name versions and meet the same FDA standards for safety, strength, and effectiveness. Yet, nearly one in three patients still hesitate to take them. Why? It’s not about science-it’s about perception.
Many patients believe generics are inferior. Some think they’re made in cheaper factories. Others worry they won’t work as well, especially for conditions like epilepsy, thyroid disease, or depression. A 2024 study found that 24.1% of patients feared generics wouldn’t control symptoms as well as brand names. Another 29.5% were scared of new or different side effects. These fears aren’t random. They come from real experiences, mixed messages, and a lack of clear communication.
The Real Story Behind Generic Drugs
Every generic drug must pass the same strict tests as its brand-name counterpart. The FDA requires proof of bioequivalence: the generic must deliver the same amount of active ingredient into the bloodstream at the same rate. That means the body absorbs it just like the brand. The acceptable range? 80% to 125%-a tight window that ensures no meaningful difference in how the drug works.
Generics aren’t copies. They’re exact matches in active ingredients, dosage form, strength, and route of administration. The only differences are in inactive ingredients-fillers, dyes, or coatings-which don’t affect how the drug works. Even the manufacturing facilities are held to the same inspections. The FDA checks generic plants as often as brand-name ones.
Take sertraline, the generic version of Zoloft. In a Reddit thread with over 1,400 comments, most users reported no difference. But a small number said they had worse side effects. What happened? Often, it’s not the drug-it’s the change. Switching from one brand to another, even if both are generic, can trigger a nocebo effect: expecting trouble makes you feel it.
Who’s Most Likely to Doubt Generics-and Why
Not everyone feels the same way about generics. Research shows clear patterns:
- Patients with low health literacy are twice as likely to believe generics are less safe or effective.
- Non-white patients report lower confidence than white patients-78.3% vs. 89.1%.
- People on Medicaid are more likely to distrust generics than those with private insurance.
- Older adults (over 60) are actually more comfortable with generics than younger people.
- Those with higher education and income trust generics more.
These aren’t just numbers. They point to deeper gaps: lack of access to clear information, mistrust in the system, or past experiences where cost-cutting felt like care-cutting. The issue isn’t the drug. It’s the message.
What Works: The 3 Most Effective Strategies
Research consistently shows that the best way to build confidence isn’t through brochures, ads, or websites. It’s through conversation.
1. Talk About It-Seriously
A 2023 study found that patients who received a 2- to 3-minute explanation from their provider or pharmacist were 21% more likely to accept a generic. The key? Not just saying, “This is cheaper.” It’s saying, “This is the same drug. The FDA requires it to work just like your old one. Here’s how we know.”
Use simple analogies: “It’s like buying store-brand aspirin instead of Bayer. Same active ingredient, same results, just less packaging.”
Don’t assume patients know what “bioequivalent” means. Say: “Your body gets the same amount of medicine, at the same speed. That’s why it works the same.”
2. Let Patients Ask Questions
Patients who feel involved in the decision are far more likely to stick with it. A 2024 FDA report found that patients who weren’t asked before switching were more likely to stop taking the medication-or blame the generic for side effects they’d had before.
Ask: “Have you taken generics before? What was your experience?”
Listen. If someone says, “I had a bad reaction,” don’t dismiss it. Ask: “Was it this exact medicine, or just a different version of it?” Sometimes, switching between two different generic manufacturers causes a perceived change-even though both are FDA-approved.
3. Use Pharmacists as Educators
Pharmacists are the most trusted source of drug information for most patients. When a pharmacist explains why a generic was substituted, 84.7% of patients felt comfortable with the switch. Without that explanation, only 63.2% did.
Good pharmacy counseling includes:
- Confirming the patient knows it’s a generic
- Explaining it’s not a downgrade
- Offering to answer questions later
- Not rushing the conversation
Walmart Pharmacy scores low on patient satisfaction for this reason. CVS Health scores higher because pharmacists take the time. It’s not about training-it’s about time.
What Doesn’t Work
Handing out pamphlets? 62% of patients say they’re “somewhat helpful at best.”
Posting signs in the waiting room? Most people don’t read them.
Just saying, “It’s cheaper” without explaining safety? That reinforces the idea that generics are a compromise.
Assuming patients know the FDA approves them? Many don’t. Only 43% of patients in one study could correctly define what the FDA does.

Special Cases: When Generics Need Extra Care
Some drugs are more sensitive to small changes in absorption. These include:
- Thyroid medications (like levothyroxine)
- Antiseizure drugs (like phenytoin)
- Immunosuppressants (like cyclosporine)
- Warfarin
- Complex delivery systems (inhalers, patches, injectables)
For these, consistency matters. Once a patient is stable on a specific generic brand, it’s best to keep them on it. Switching between generic manufacturers can cause small fluctuations-even if both are FDA-approved.
Doctors and pharmacists should document which generic version a patient is on and avoid unnecessary switches. If a change is needed, explain why and monitor closely.
How to Start Today
You don’t need a big budget or new software. Start small:
- Train staff to use a 30-second script: “This is a generic version of your medicine. It has the same active ingredient and works the same way. The FDA makes sure it’s just as safe and effective.”
- Ask patients: “Do you have any concerns about switching to a generic?”
- Keep a simple handout ready with the FDA’s top 5 facts about generics (e.g., “Generics must be identical in strength, dosage, and safety”).
- Track patient feedback. If someone says, “It didn’t work,” find out why. Was it a new generic? A different pill shape? A change in routine?
One clinic in Ohio started using a 2-minute script during check-out. Within six months, generic acceptance rose from 71% to 92%. No new tools. Just better talk.
The Bigger Picture
Generic drugs save the U.S. healthcare system over $370 billion a year. That’s money that keeps premiums low, expands access, and funds new treatments. But that value disappears if patients don’t trust them.
Building confidence isn’t about marketing. It’s about respect. It’s about recognizing that patients care deeply about their health-and they deserve clear, honest answers.
The science is solid. The savings are real. What’s missing is the conversation. Start talking. Listen. Then watch confidence grow.



Comments (15)