When a pharmacist hands a patient a generic pill instead of the brand-name drug their doctor prescribed, it’s not just a cost-saving move-it’s a legal decision. In the U.S., pharmacists are the final checkpoint in the generic substitution system, and they carry real legal responsibility for getting it right. One wrong move can lead to disciplinary action, patient harm, or even lawsuits. Understanding what you can and cannot do when dispensing generics isn’t optional-it’s part of your job.
What Counts as a Legal Generic?
Not every generic drug is legally interchangeable. The FDA’s Orange Book is the official source that lists which generics are rated as therapeutically equivalent to their brand-name counterparts. Only drugs marked with an "A" rating are approved for automatic substitution. An "A" rating means the generic has the same active ingredient, strength, dosage form, and route of administration as the brand, and it’s been proven to work the same way in the body.But here’s what many don’t realize: just because a drug is generic and cheap doesn’t mean it’s legally substitutable. Some generics get an "B" rating-meaning they’re not considered bioequivalent-and those can’t be substituted under any state law. Pharmacists must check the Orange Book every time they fill a prescription. It’s updated monthly, and relying on memory or outdated software is a common mistake that leads to violations.
State Laws Vary-A Lot
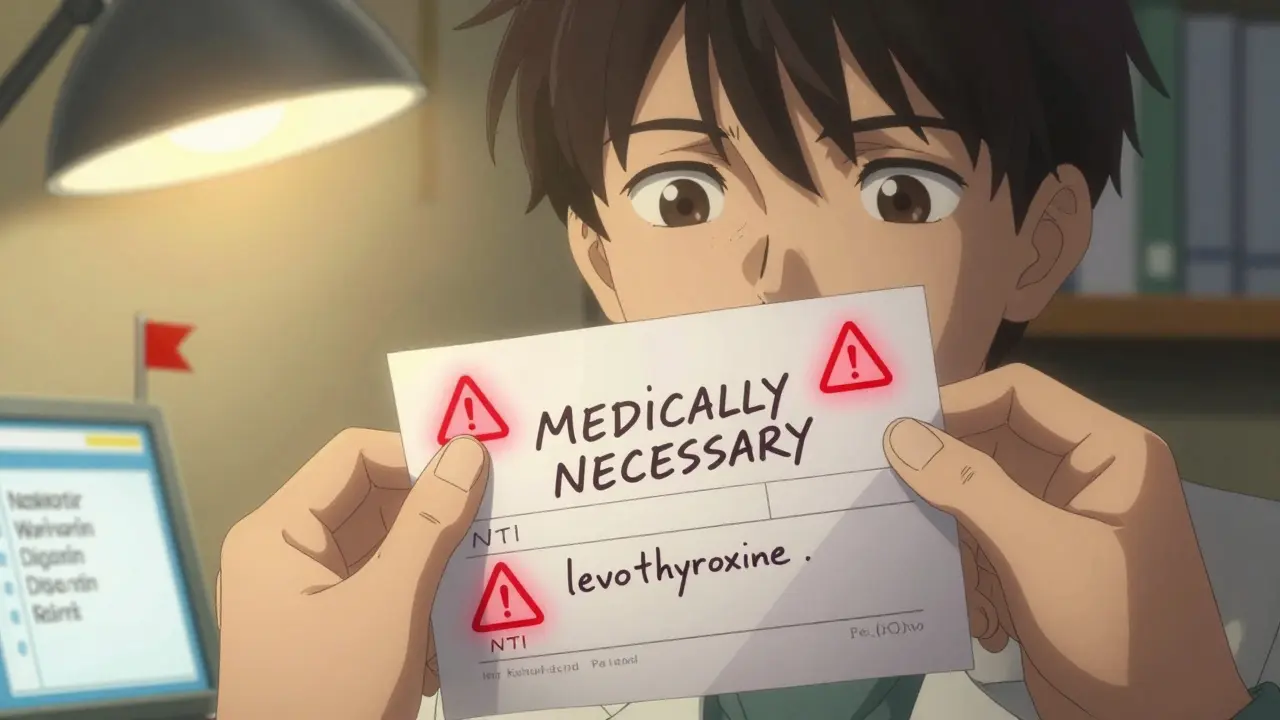
There’s no single federal rule that tells pharmacists when to substitute. Instead, each of the 50 states and D.C. has its own laws, and they don’t all match up. Some states require substitution unless the prescriber says "do not substitute." Others let pharmacists decide. And some states have special rules for certain drugs.For example, in Tennessee, it’s illegal to substitute any generic for antiepileptic drugs if the patient has epilepsy or seizures-even if the generic has an "A" rating. In Hawaii, you need both the prescriber’s and patient’s written consent before substituting epilepsy meds. In Florida, you can’t substitute any drug classified as having a narrow therapeutic index-like warfarin, digoxin, or levothyroxine-unless the prescriber explicitly writes "MEDICALLY NECESSARY" by hand on the prescription. That phrase has to be handwritten. Typing it into an electronic system doesn’t count.
Thirty-two states require you to get the patient’s explicit consent before substituting. Eighteen others operate on presumed consent-you can swap the drug unless the patient says no. That means in New York, you can substitute without asking. In California, you have to tell the patient and get their okay. Mixing these up is one of the top reasons pharmacists get cited by state boards.
What You Must Document
Documentation isn’t just paperwork-it’s your legal shield. If a patient has an adverse reaction after a substitution, and you didn’t document consent or the prescriber’s "medically necessary" note, you’re exposed. State boards of pharmacy report that 68% of all substitution-related disciplinary actions in 2022 were due to poor documentation.You need to record:
- Which drug was dispensed (brand or generic)
- Whether substitution occurred
- Whether patient consent was obtained (and how-verbal, written, electronic)
- Any prescriber notation like "do not substitute" or "medically necessary"
- The date and time of the transaction
Electronic health record systems can help, but they’re not foolproof. If your pharmacy’s software doesn’t auto-flag a "medically necessary" prescription from Florida, you’re still responsible. Always double-check the prescription label and the prescriber’s notes before dispensing.
Drugs You Can’t Substitute-Even If They’re "A-Rated"
Some drugs are so sensitive that even FDA-approved generics can’t be swapped without risking patient safety. These are called narrow therapeutic index (NTI) drugs. A small change in blood levels can mean the difference between therapeutic effect and toxicity.Common NTI drugs include:
- Warfarin (blood thinner)
- Digoxin (heart medication)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine (anti-seizure meds)
- Cyclosporine (immunosuppressant)
A 2019 study in JAMA Internal Medicine found that substituting certain cardiac glycosides-even when labeled "A-rated"-led to a 12.7% increase in adverse events. That’s why states like Florida, California, and New York have extra rules for these drugs. Even if the law allows substitution, best practice is to avoid it unless the prescriber specifically approves.
When Patients Ask: How to Talk About Substitution
Patients often don’t understand why a generic looks different or costs less. And when they have a bad experience-like a seizure or a blood clot-they blame the pharmacist, not the system.Here’s what works:
- "This generic has been approved by the FDA to work exactly like the brand. It’s the same medicine, just cheaper. We’re required by law to offer it unless your doctor says otherwise."
- "Some medications, like your thyroid pill, need to stay the same brand because even small changes can affect how your body responds. Your doctor wrote ‘do not substitute’-so we’re keeping you on the brand."
- "You have the right to ask for the brand name. We can fill it, but you’ll pay more. Would you like to go ahead?"
Studies show patients are 78% more satisfied when they’re clearly told why a substitution happened. But 63% of negative reviews cite "no explanation" as the main reason for dissatisfaction. Your communication isn’t just nice-it’s part of your legal duty to prevent harm.

What Happens If You Get It Wrong?
The consequences aren’t theoretical. In 2023, a pharmacist in Tennessee was suspended for six months after substituting a generic antiepileptic for a patient with epilepsy. The patient had a seizure and was hospitalized. The pharmacist didn’t know about Tennessee’s specific ban-despite it being on the state board’s website for over a decade.Possible penalties include:
- License suspension or revocation
- Fines up to $10,000 per violation
- Mandatory continuing education
- Malpractice lawsuits
And it’s not just the pharmacist. The pharmacy owner can be held liable too. Many chains now require staff to complete state-specific substitution training every year. In 2022 alone, 17 states changed their substitution laws. Keeping up isn’t optional-it’s survival.
How to Stay Compliant
Here’s what you need to do daily:- Check the FDA Orange Book for the drug’s therapeutic equivalence rating before dispensing.
- Verify the prescription for "do not substitute," "medically necessary," or other restrictions.
- Know your state’s consent rules-explicit or presumed?
- Document every substitution decision in the pharmacy system.
- When in doubt, call the prescriber. Better safe than sorry.
Use tools like state pharmacy board websites, NABP’s model substitution act, and your pharmacy’s compliance software. But never rely on them alone. Your professional judgment is the last line of defense.
What’s Changing in 2026?
The FDA now requires all generic drug labels to include a clear statement: "This product is approved as interchangeable with the brand-name drug." That change, mandated by the 2022 Consolidated Appropriations Act, went into full effect at the end of 2024. It’s meant to reduce patient confusion.Also, 19 states are updating their laws to include biosimilars-biologic drugs that are similar to, but not exact copies of, brand-name biologics. These have different substitution rules than traditional generics, and pharmacists need to know the difference.
The bottom line? Generic substitution saves the U.S. healthcare system over $300 billion a year. But it only works if pharmacists follow the law. Your job isn’t just to fill prescriptions-it’s to protect patients from legal and clinical risks that come with substitution. Get it right, every time.
Can a pharmacist substitute a generic drug without the patient’s permission?
It depends on the state. In 32 states, pharmacists must get the patient’s explicit consent before substituting a generic. In 18 states, consent is presumed-meaning substitution is allowed unless the patient objects. Always check your state’s pharmacy board rules. Even in presumed consent states, best practice is to inform the patient to avoid complaints or misunderstandings.
Are all generic drugs safe to substitute?
No. Only generics with an "A" rating in the FDA’s Orange Book are approved for substitution. Even then, some drugs-like warfarin, levothyroxine, and antiepileptics-are considered high-risk due to their narrow therapeutic index. Many states ban substitution for these, regardless of FDA rating. Pharmacists must know both the FDA classification and their state’s specific restrictions.
What does "medically necessary" mean on a prescription?
"Medically necessary" is a legal term used by prescribers to prevent generic substitution. In states like Florida and New York, this phrase must be handwritten on the prescription by the doctor. Typing it into an electronic system doesn’t count. If it’s not handwritten, the pharmacist is legally allowed to substitute the generic-even if the drug is on a restricted list. This rule exists to ensure the prescriber actively chose to block substitution.
Can I be held liable if a patient has a bad reaction after a generic substitution?
Yes. If you substituted a drug without following your state’s laws-like skipping consent, ignoring a "do not substitute" note, or substituting a restricted drug-you can be held legally responsible. Even if the FDA says the generic is equivalent, state law and patient safety come first. Documentation is your best defense. If you followed every rule and still had an issue, liability is less likely.
How often do state laws on generic substitution change?
Frequently. In 2022 alone, 17 states updated their generic substitution laws. Changes include new restrictions on NTI drugs, updates to consent requirements, and new rules for biosimilars. Pharmacists should check their state board’s website quarterly and complete at least 40 hours of continuing education annually focused on pharmacy law and regulation.


Comments (8)