SGLT2 Inhibitor Risk Assessment Tool
Understanding Your Risk
SGLT2 inhibitors can cause euglycemic diabetic ketoacidosis (euDKA) even when blood sugar is normal. This tool helps you assess your risk based on symptoms, blood sugar levels, and other factors.
The article explains that euDKA is dangerous because it's often missed when blood sugar is below 250 mg/dL. Early detection is critical.
Risk Assessment
What to do next:
Key Information
According to the article, euDKA can occur with blood sugar below 250 mg/dL. Symptoms like nausea, vomiting, and abdominal pain should never be ignored.
If you have moderate or high ketone levels, you should seek immediate medical attention even if your blood sugar is normal.
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar, protects your heart, and helps your kidneys is a big win. That’s why SGLT2 inhibitors like canagliflozin, dapagliflozin, and empagliflozin became so popular. But there’s a quiet danger hiding in plain sight: a rare but deadly form of diabetic ketoacidosis that doesn’t look like the classic version you learned about in medical school.
What Makes SGLT2 Inhibitors Different
SGLT2 inhibitors work by making your kidneys flush out extra sugar through urine. It’s a clever trick-instead of forcing your body to use more insulin, you’re just getting rid of the excess glucose. This lowers blood sugar without causing low blood sugar episodes, which is why many patients and doctors like them. They also reduce heart failure hospitalizations and slow kidney decline, something no other diabetes drug class has done as consistently. But here’s the catch: when your body starts burning fat for fuel because glucose isn’t getting into cells efficiently, it produces ketones. Normally, that’s fine. But with SGLT2 inhibitors, the system gets thrown off balance. Even when blood sugar is only mildly high-or even normal-you can still develop ketoacidosis. This is called euglycemic diabetic ketoacidosis, or euDKA.Euglycemic DKA: The Silent Threat
Traditional diabetic ketoacidosis (DKA) shows up with blood sugar over 250 mg/dL, fruity breath, vomiting, and confusion. It’s obvious. euDKA? Not so much. Blood sugar might be 150 mg/dL or even lower. A patient feels nauseous, tired, or has stomach pain. They check their glucose-"It’s not that high," they think-and delay care. By the time they get to the ER, they’re in critical condition. The European Medicines Agency (EMA) confirmed this in June 2023 after reviewing over 100 cases. They found that nearly half of all DKA events linked to SGLT2 inhibitors had blood sugar under 250 mg/dL. In some cases, it was below 200 mg/dL. That’s why doctors now say: if you’re on one of these drugs and feel unwell, don’t wait for high glucose to act.Who’s Most at Risk
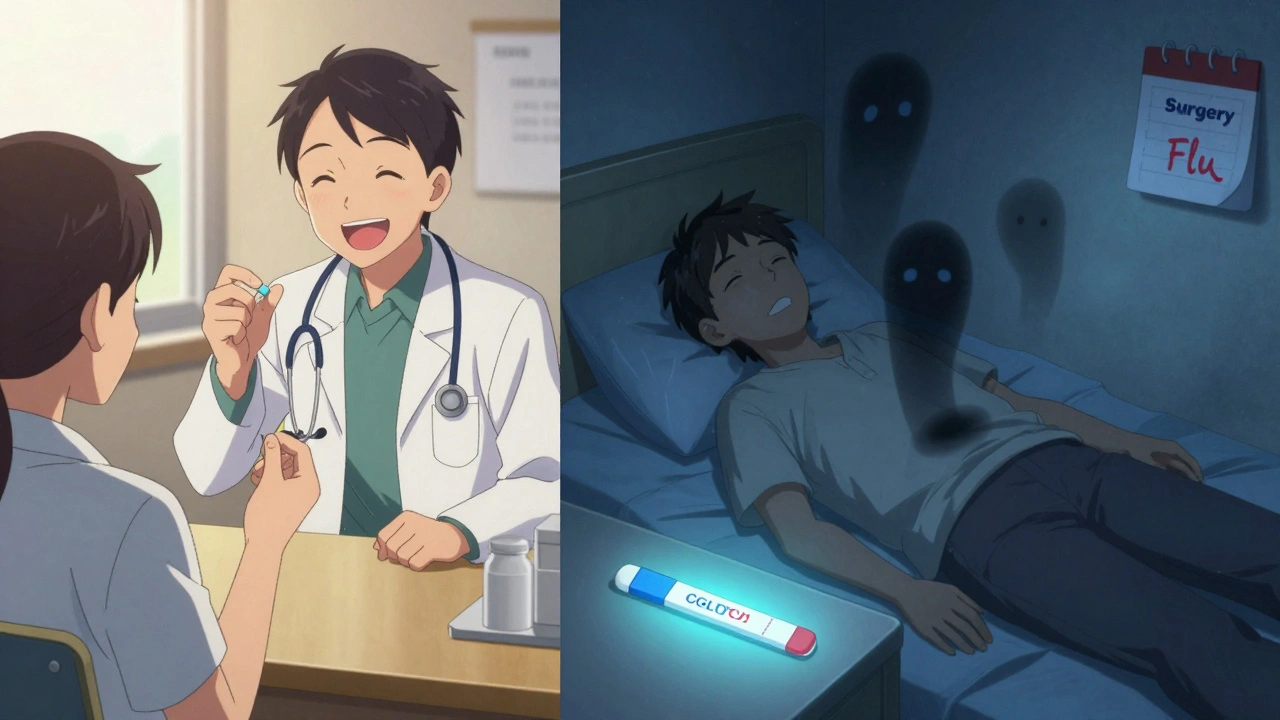
Not everyone on SGLT2 inhibitors gets euDKA. But certain situations make it far more likely:- Illness-Infections, flu, or even a bad cold can trigger it. Your body goes into stress mode, releases counter-regulatory hormones, and ketone production spikes.
- Surgery or fasting-If you’re told to stop eating before a procedure, your body switches to fat-burning mode. SGLT2 inhibitors keep pushing glucose out, making ketones pile up faster.
- Insulin reduction-People with type 2 diabetes who’ve been on insulin for years and then switch to an SGLT2 inhibitor sometimes cut their insulin too much. That’s dangerous.
- Low insulin production-If your pancreas can’t make enough insulin (low C-peptide), you’re at higher risk. One study found 2.4% of users with C-peptide under 1.0 ng/mL developed DKA, compared to 0.6% in those with higher levels.
- Alcohol binges-Heavy drinking suppresses liver glucose production and increases fat breakdown, creating the perfect storm.

The Numbers Don’t Lie
Let’s put this in perspective. The overall risk is low-about 0.1 to 0.5 cases per 100 patients per year. That’s rare. But compared to people not taking SGLT2 inhibitors, the risk is nearly three times higher. A 2024 study in Metabolites tracked over 350,000 people and found 2.03 DKA events per 1,000 person-years with SGLT2 inhibitors, versus 0.75 with DPP-4 inhibitors. And here’s the scary part: mortality is higher. One 2021 study found a 4.3% death rate in SGLT2-related DKA cases, compared to 2.1% in traditional DKA. Why? Because it’s missed. Emergency room staff aren’t looking for ketoacidosis when glucose is normal. By the time ketones are detected, the acidosis is severe.What Doctors Are Doing About It
Guidelines have changed. The American Diabetes Association, the Endocrine Society, and the European Association for the Study of Diabetes all agree on the same steps:- Stop SGLT2 inhibitors at least 3 days before surgery or any procedure requiring fasting.
- Hold the drug during serious illness-fever, infection, vomiting, or diarrhea.
- Check ketones if you feel unwell, even if your blood sugar is under 250 mg/dL.
- Don’t restart the drug until you’re fully recovered and ketones are gone.
Who Should Avoid These Drugs
Some people shouldn’t take SGLT2 inhibitors at all:- People with type 1 diabetes (unless under strict supervision and with insulin)
- Those with a past history of DKA
- Patients with very low insulin production (C-peptide < 1.0 ng/mL)
- Anyone with chronic alcohol use or eating disorders
- People with severe kidney disease (eGFR < 30)
What You Can Do Right Now
If you’re on an SGLT2 inhibitor:- Ask your doctor if you have low insulin production. A simple C-peptide test can help.
- Keep ketone strips at home. Urine strips are cheap and easy. Blood ketone meters are more accurate but cost more.
- Know the symptoms: nausea, vomiting, abdominal pain, unusual fatigue, trouble breathing, confusion.
- If you feel sick, check your ketones. If they’re moderate or high, go to the ER-even if your blood sugar is normal.
- Never stop insulin or cut your dose without talking to your provider.
The Bigger Picture
Yes, SGLT2 inhibitors save lives. They reduce heart attacks, hospitalizations for heart failure, and slow kidney failure. For many people, the benefits far outweigh the risks. But risk doesn’t disappear just because it’s rare. The key is awareness. Newer drugs like ertugliflozin and dual SGLT1/2 inhibitors like licogliflozin (currently in trials) may have lower DKA risk. But for now, the same rules apply. The future is moving toward risk prediction. A 2024 study in Lancet Digital Health built a machine learning model that uses 15 factors-like age, kidney function, insulin use, and prior infections-to predict who’s most likely to develop euDKA. It was 87% accurate. Soon, doctors may be able to screen patients before prescribing these drugs.Final Thoughts
SGLT2 inhibitors are powerful tools. But they’re not magic. They come with a hidden risk that’s easy to miss. If you’re taking one, don’t assume your blood sugar is the only warning sign. Learn the symptoms. Keep ketone strips handy. Talk to your doctor about your personal risk. And if you ever feel off-don’t wait. Check your ketones. Go to the hospital. Your life could depend on it.Can SGLT2 inhibitors cause diabetic ketoacidosis even if my blood sugar is normal?
Yes. This is called euglycemic diabetic ketoacidosis (euDKA). Blood sugar may be below 250 mg/dL, sometimes even under 200 mg/dL, while ketones build up and blood becomes acidic. It’s dangerous because it’s easily missed-many patients and even some doctors don’t suspect DKA without high glucose.
How common is DKA with SGLT2 inhibitors?
It’s rare-about 0.1 to 0.5 cases per 100 patients per year. But compared to other diabetes medications, the risk is nearly three times higher. Most cases happen within the first year of use, often triggered by illness, surgery, or reduced food intake.
Should I stop taking my SGLT2 inhibitor if I get sick?
Yes. If you have an infection, fever, vomiting, or diarrhea, stop your SGLT2 inhibitor and contact your doctor. Your body is under stress and more likely to produce ketones. Restart the medication only after you’ve recovered and ketone levels are normal.
Do I need to check ketones regularly?
Not every day-but always when you’re ill, before surgery, or if you feel unwell (nausea, stomach pain, fatigue). Keep urine or blood ketone strips on hand. If ketones are moderate or large, seek medical help immediately, even if your blood sugar is normal.
Are SGLT2 inhibitors safe for people with type 1 diabetes?
Generally, no. They are not approved for type 1 diabetes in most countries. However, in rare cases under strict supervision, they may be used with insulin-but only if the patient is trained to monitor ketones and understands the risks. The risk of DKA is significantly higher in type 1 users.
What are the signs I should go to the ER?
Go to the ER if you have nausea/vomiting, abdominal pain, rapid breathing, confusion, extreme fatigue, or fruity-smelling breath-even if your blood sugar is below 250 mg/dL. These are signs of ketoacidosis. Don’t wait for high glucose. Early treatment saves lives.
Can I restart my SGLT2 inhibitor after a DKA episode?
Usually not. Once you’ve had DKA while on an SGLT2 inhibitor, most doctors recommend avoiding these drugs permanently. The risk of recurrence is too high. Alternative medications like GLP-1 agonists or DPP-4 inhibitors are safer options.
Do all SGLT2 inhibitors carry the same risk?
The risk appears similar across all drugs in this class-canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin. Higher doses (like canagliflozin 300 mg) may slightly increase risk, but the mechanism is the same. No SGLT2 inhibitor is considered "safe" from this risk.



Comments (9)