Antihistamine Selection Guide
Find Your Best Antihistamine
Answer a few questions about your priorities to see which antihistamine might work best for you.
How important is avoiding drowsiness?
How severe is your itching?
How quickly do you need relief?
Your Recommended Antihistamine
Based on your answers, this antihistamine is the best match for your priorities.
Important Considerations
Remember, antihistamines work best when taken daily. If you don't see relief after 2-4 weeks, consult your doctor about dose adjustment or alternative treatments. Never double up on first-generation antihistamines like Benadryl with second-generation ones.
When hives show up-sudden red, itchy welts that seem to appear out of nowhere-you want relief, fast. Antihistamines are the go-to solution, but not all are the same. Some knock you out. Others barely touch the itching. And for many people, even the strongest ones stop working after a while. If you’ve been stuck in a cycle of taking pills that don’t help, or waking up groggy because of them, you’re not alone. About 20% of people get hives at least once in their life. For 1 in 100, it becomes chronic, lasting six weeks or longer. The good news? There’s a clear path forward, and it starts with understanding which antihistamine is right for you-and when it’s time to try something else.
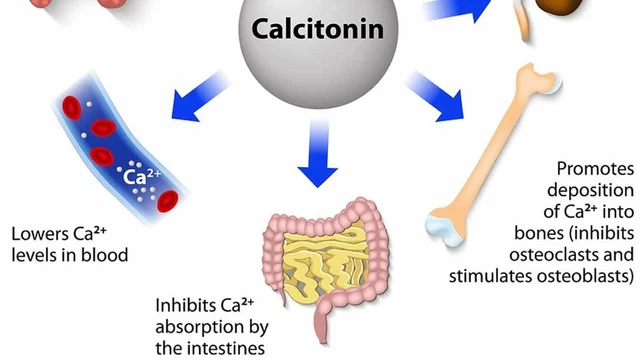
How Antihistamines Stop Hives
First-Generation vs. Second-Generation: The Drowsiness Divide
Not all antihistamines are created equal. The older ones-like diphenhydramine (Benadryl)-were groundbreaking when they came out in the 1940s. They block histamine, the chemical that triggers hives, but they also cross into your brain. That’s why about half of people who take them feel drowsy, dizzy, or foggy. These effects aren’t just annoying-they can be dangerous. The FDA requires boxed warnings on first-generation antihistamines for impaired driving and increased fall risk in older adults.
Second-generation antihistamines were designed to fix that. Drugs like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were developed in the 1990s to stay out of the brain. They’re just as good at stopping hives, but with far less sedation. Studies show only 10-15% of people feel sleepy on these, compared to nearly 50% on Benadryl. That’s why doctors now recommend them as the first step for every case of hives, acute or chronic.
Which Second-Generation Antihistamine Is Best?
There’s no single “best” antihistamine for everyone. But data shows clear differences in how they perform.
Cetirizine (Zyrtec) works fast-peak levels in the blood within an hour. In clinical trials, it reduced itching by 78% in chronic hives patients, more than any other second-generation option. But it’s also the most likely to cause drowsiness among the non-sedating group-about 15% of users report feeling tired. If you’re looking for maximum itch control and don’t mind a little sleepiness, this is the strongest option.
Loratadine (Claritin) is milder. It takes about an hour and a half to kick in and reduces itching by about 65%. It’s the least likely to cause drowsiness (only 8-10% of users), making it a solid pick for daytime use. But if your hives are severe, it might not be enough.
Fexofenadine (Allegra) has the longest half-life-14 hours-and the lowest rate of drowsiness (under 10%). In driving simulations, only 8% of users showed cognitive impairment, compared to 15% on cetirizine. If you drive, work with machines, or need to stay sharp, this is the safest choice. It’s also the least likely to interact with food-unlike cetirizine, which works better on an empty stomach.
Here’s how they stack up:
| Medication | Standard Dose | Onset of Action | Drowsiness Rate | Itch Reduction | Best For |
|---|---|---|---|---|---|
| Cetirizine (Zyrtec) | 10 mg daily | 1 hour | 15% | 78% | Severe itching, fast relief |
| Loratadine (Claritin) | 10 mg daily | 1.3 hours | 10% | 65% | Mild hives, daytime use |
| Fexofenadine (Allegra) | 180 mg daily | 2.6 hours | 8% | 70% | Driving, work, low drowsiness |
Real-world reviews back this up. On DrugReview.com, cetirizine has a 3.7/5 rating with 52% saying it works-but 38% report drowsiness. Fexofenadine scores 3.3/5, with 45% effectiveness but only 22% reporting tiredness. If you’re choosing based on experience, fexofenadine gives you the best balance of relief and alertness.

What If Your Antihistamine Stops Working?
Many people hit a wall. You take your daily pill. The hives come back. You double the dose. Still no relief. You’re not broken-you’re normal. Clinical studies show that standard-dose second-generation antihistamines control symptoms in only 43% of chronic hives patients. That means more than half need more.
The solution isn’t switching brands. It’s increasing the dose. The 2023 International Consensus Guidelines say it’s safe to go up to four times the standard dose. That means 40 mg of cetirizine, 40 mg of loratadine, or 720 mg of fexofenadine per day. Studies show this boosts effectiveness to 70-75% for most people. It’s not experimental-it’s standard care.
But here’s the catch: you can’t just start taking more on your own. High doses carry a small risk of heart rhythm changes, especially if you have existing heart conditions or take other medications. Always talk to your doctor before increasing your dose. They’ll check your heart rhythm and make sure it’s safe.
Alternatives When Antihistamines Fail
If even four times the dose doesn’t help, you’re not out of options. There are three proven next steps:
- Omalizumab (Xolair): This is a monthly injection, originally for asthma, now approved for chronic hives that don’t respond to antihistamines. In trials, it cleared symptoms completely in 58% of patients. But it costs about $3,200 per shot. Insurance usually covers it if you’ve tried high-dose antihistamines first.
- Ligelizumab: A newer drug, still in phase 3 trials, but already showing promise. In early studies, it worked better than omalizumab-51% complete response versus 26%. The FDA gave it Breakthrough Therapy status in March 2023. It could be available by late 2025.
- Cyclosporine: An immune suppressant used for severe cases. It works in about 65% of patients, but it can damage your kidneys over time. Doctors only use it for short bursts-usually 3-6 months-because of the risks.
Other options like leukotriene blockers (montelukast) or doxepin (a low-dose antidepressant) are sometimes added, but they’re less effective. Biologics like omalizumab and ligelizumab are becoming the gold standard for treatment-resistant hives.
How to Track Your Hives and Find Triggers
Medication isn’t the whole story. Many people with chronic hives have triggers they don’t realize are causing flare-ups. Common ones include:
- NSAIDs (ibuprofen, naproxen)-triggered in 32% of patients
- Stress-reported by 28%
- Heat or sweating-24%
- Alcohol and certain foods-18%
Tracking your symptoms daily makes a huge difference. The Urticaria Activity Score (UAS) is a simple tool: rate your itching (0-3) and number of hives (0-3) each day. Add them up. If your score stays above 6 for more than a week, your treatment isn’t working.
Apps like Hive Wise help you log symptoms, medication times, and potential triggers. People who use them are 78% more likely to identify patterns and reduce flare-ups. One user on Reddit found her hives flared every time she ate tomatoes. Another realized her stress spikes came after weekend work calls. Small changes, big results.
When to See a Specialist
Most primary care doctors start you on antihistamines. But only 32% feel confident handling cases that don’t respond. That’s why 68% of patients with chronic hives are referred to allergists or dermatologists.
You should see a specialist if:
- Your hives last more than six weeks
- Standard or high-dose antihistamines don’t help
- You have swelling in your throat, tongue, or lips (angioedema)
- You’re considering biologics or immunosuppressants
Specialists can run blood tests to check for autoimmune causes-like thyroid disease-which doubles your risk of treatment failure. They can also test for high-sensitivity C-reactive protein (hs-CRP). If your level is above 3 mg/L, you’re 78% more likely to need something stronger than antihistamines.
What’s Next for Hives Treatment
The future is personal. Researchers are looking at genetic testing to predict which antihistamine will work best for you. A 2024 study found that 22% of people have a gene variation (CYP2C19) that makes cetirizine less effective. In five years, a simple blood test could tell you whether to start with fexofenadine instead.
Meanwhile, new mast cell stabilizers are in clinical trials. These drugs stop hives at the source-by preventing mast cells from releasing histamine in the first place. If they work, they could replace antihistamines entirely for some people.
For now, the best strategy is simple: start with a second-generation antihistamine, take it daily (not as needed), and give it time. If it doesn’t work, increase the dose under medical supervision. If that still fails, biologics like omalizumab or the upcoming ligelizumab can change your life. You don’t have to live with hives. There’s a plan-and it’s more effective than ever.
Can I take two different antihistamines together for hives?
Yes, but only under a doctor’s supervision. Combining cetirizine and fexofenadine is a common strategy for stubborn hives. Studies show this dual approach improves symptom control by 20-30% compared to one drug alone. But never mix first-generation antihistamines like Benadryl with second-generation ones-it increases drowsiness and risk of side effects without added benefit.
Why do my hives come back even when I take antihistamines every day?
Chronic hives are often driven by immune system activity, not just allergies. Even if you’re blocking histamine, your body may be releasing more than the drug can handle. That’s why standard doses only work in 43% of cases. Increasing to four times the dose helps 30% of those patients. If you’re still breaking out, you likely need a biologic like omalizumab or a different type of treatment.
Is it safe to take high-dose antihistamines long-term?
For most people, yes. Studies tracking patients on 40 mg of cetirizine daily for up to two years show no major safety issues. The FDA has approved dose escalation for chronic hives. The only risks are rare heart rhythm changes (0.2% of cases) and mild dry mouth or headaches. Your doctor will monitor you if you’re on high doses, especially if you have heart disease or take other medications.
Do natural remedies like quercetin or vitamin C help with hives?
There’s no strong evidence. Some people report feeling better, but no clinical trial has proven they reduce hives more than a placebo. Quercetin is a natural antihistamine, but it’s poorly absorbed by the body. You’d need to take grams per day to match the effect of 10 mg of cetirizine-and even then, it’s not reliable. Stick with proven treatments first.
Can stress really make hives worse?
Absolutely. Stress doesn’t cause hives, but it can trigger flare-ups in people with chronic spontaneous urticaria. Studies show stress hormones like cortisol can activate mast cells, releasing more histamine. Managing stress with sleep, exercise, or therapy doesn’t cure hives-but it can reduce how often they show up. Many patients report fewer outbreaks after starting mindfulness or yoga.
What to Do Next
If you’re still dealing with hives:
- Switch to a second-generation antihistamine if you’re still using Benadryl or similar.
- Take it daily, not just when you feel itchy.
- Use a symptom tracker for two weeks-note timing, food, stress, and temperature.
- If symptoms persist after 2-4 weeks, ask your doctor about increasing the dose.
- If you’re still not better after fourfold dosing, request a referral to an allergist or dermatologist.
You don’t have to suffer. Hives are frustrating, but they’re treatable. The tools to control them exist-you just need the right plan.


Comments (14)