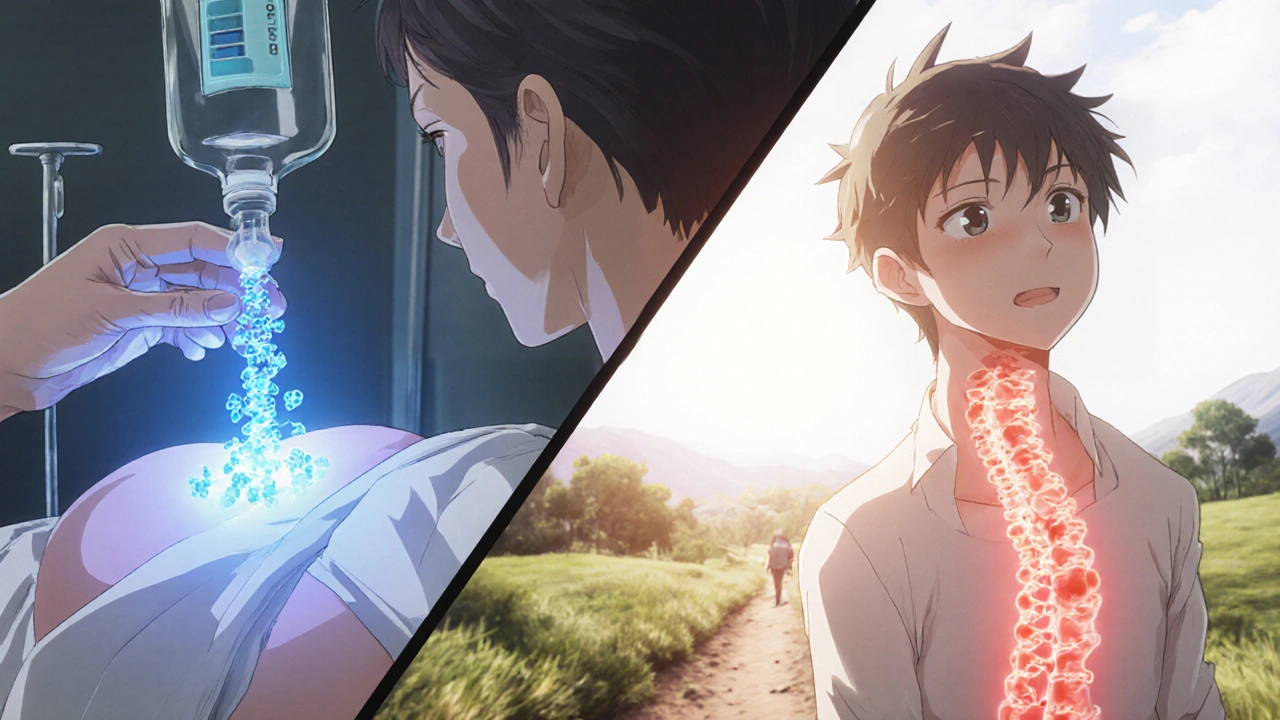
Chronic back pain that doesn’t go away with rest? Morning stiffness so bad it takes an hour to get out of bed? If you’ve been told you have ankylosing spondylitis (AS), you know it’s not just ordinary back pain. It’s inflammation deep in your spine and sacroiliac joints - a slow, invisible force that can fuse vertebrae together over time. For decades, people with AS had few options beyond NSAIDs and physical therapy. But since the early 2000s, a new class of drugs has changed everything: TNF inhibitors.
What Exactly Is Ankylosing Spondylitis?
Ankylosing spondylitis isn’t just back pain. It’s an autoimmune disease where the immune system attacks the spine and joints, triggering inflammation that doesn’t turn off. Over years, this inflammation leads to bone erosion, then abnormal bone growth - fusing vertebrae into a rigid, inflexible column. The term comes from Greek: ankylos means stiff or bent, and spondylos means spine.
It often starts in young adults, between ages 17 and 45. Men are affected more often than women, but women tend to have milder symptoms that are harder to diagnose. The biggest red flag? Pain that improves with movement and gets worse with rest. Morning stiffness lasting more than 30 minutes is a classic sign. Many people mistake it for a herniated disc or muscle strain - and wait years before getting the right diagnosis.
Genetics play a big role. About 90% of people with AS carry the HLA-B27 gene. But having the gene doesn’t mean you’ll get the disease - only 5-6% of HLA-B27-positive people develop AS. Other factors like gut bacteria and immune triggers are likely involved. Diagnosis relies on imaging (X-rays or MRI showing sacroiliitis) and blood tests for inflammation markers like CRP and ESR.
Why TNF Is the Key Target
At the heart of AS is a protein called tumor necrosis factor-alpha (TNF-α). It’s a signaling molecule your immune system uses to call for help during infection or injury. In AS, this signal gets stuck on - flooding the spine and joints with inflammation.
Studies show TNF-α is found in high levels in the sacroiliac joints of AS patients. It activates other immune cells, increases pain signals, and directly contributes to bone damage. MRI scans of untreated AS patients show bright spots in the spine - signs of active inflammation. After starting a TNF inhibitor, those spots fade within weeks.
Before TNF inhibitors, treatment was mostly about managing pain. Now, these drugs actually change the disease course. They reduce inflammation so much that many patients can return to work, exercise, and daily life without constant pain.
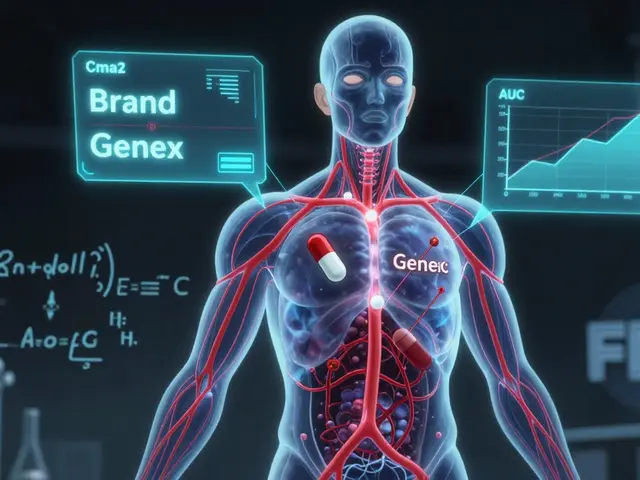
The Five TNF Inhibitors Approved for AS
Five TNF blockers are currently approved in the U.S. for ankylosing spondylitis. They all block TNF-α, but they work differently and are given in different ways.
- Infliximab (Remicade): Given by IV infusion every 4-8 weeks. Requires a clinic visit. First approved for AS in 2003.
- Etanercept (Enbrel): Injected under the skin twice a week. One of the most studied and longest-used options.
- Adalimumab (Humira): Injected under the skin every other week. Popular for its convenience and strong results.
- Certolizumab pegol (Cimzia): Injected under the skin every 2 weeks or weekly. Unique because it doesn’t contain a part of the antibody that can trigger immune reactions.
- Golimumab (Simponi): Injected under the skin once a month. One of the few options with monthly dosing.
Each has its pros and cons. Infliximab works quickly but requires clinic visits. Adalimumab and etanercept are easy to self-administer at home. Golimumab’s monthly schedule suits people who want less frequent injections. Clinical trials show all five achieve a 58-65% response rate (ASAS20) within 12-24 weeks - meaning most patients feel at least 20% better in pain, stiffness, and function.
Who Benefits Most From TNF Inhibitors?
Not everyone with AS responds the same way. Doctors look for specific signs to predict who will do best:
- BASDAI score of 4 or higher (measures disease activity)
- Spinal pain score of 4 or higher on a 10-point scale
- CRP level above 5 mg/L or ESR above 20 mm/h
- Duration of symptoms less than 10 years
- Age under 40
One study found that if both CRP and SAA (serum amyloid A) were elevated, there was an 81% chance of a strong response to TNF inhibitors. That’s why blood tests matter - they’re not just for diagnosis, they’re predictors of treatment success.
Patients who’ve tried at least two NSAIDs at full doses for 4 weeks and still have active symptoms are the ideal candidates. Guidelines from EULAR and ASAS are clear: if NSAIDs aren’t enough, it’s time to consider a biologic.
Real Results: What Patients Actually Experience
Surveys of thousands of AS patients show consistent outcomes:
- 78% report substantial improvement in symptoms within 3 months
- 62% cut their morning stiffness from over an hour to under 30 minutes
- 85% notice relief after just 2-3 injections or infusions
- 79% maintain improvement for years, according to long-term cohort studies
One patient in the Leeds cohort went from a BASDAI score of 8.2 to 3.1 in 8 weeks on etanercept. Another switched from infliximab to adalimumab after developing psoriasis - a known side effect that sometimes appears after starting TNF blockers.
But improvement isn’t always linear. Some people feel better quickly. Others take up to 12 weeks to see full effects. Patience is key. And if one drug doesn’t work, switching to another TNF inhibitor often does - about 30-40% of patients respond to a second TNF drug after the first fails.
Side Effects and Risks
TNF inhibitors are powerful, but they come with risks. Because they suppress part of the immune system, infections become more likely.
- **Serious infections**: Tuberculosis (TB) reactivation is the biggest concern. All patients must be screened with a TB skin test or blood test before starting.
- **Skin reactions**: Psoriasis or rashes can appear - sometimes improving, sometimes worsening.
- **Injection site reactions**: Redness, itching, or swelling at the injection site (reported in 19% of users).
- **Upper respiratory infections**: Common, but usually mild.
- **Heart failure**: Worsening in people with existing heart conditions.
- **Cancer risk**: No increased risk of most cancers, including lymphoma, based on long-term data from the British Society for Rheumatology.
The FDA requires a black box warning for all TNF inhibitors about serious infections, cancer, and heart failure. But real-world data from over 20 years of use shows these risks are low for most people - especially when screened and monitored properly.
Cost, Access, and Biosimilars
TNF inhibitors are expensive. Humira alone cost over $21 billion globally in 2022. But prices are dropping thanks to biosimilars - drugs that are nearly identical to the original biologics.
Amjevita, a biosimilar to Humira, entered the U.S. market in 2017 and now holds 32% of the adalimumab market. Biosimilars cost 15-20% less and are just as safe and effective. In the UK and Germany, 65-70% of eligible AS patients get TNF inhibitors within two years of diagnosis. In the U.S., that number is only 45-50% - mostly because of insurance hurdles.
Many specialty pharmacies now offer financial assistance, co-pay cards, and 24/7 nursing support for self-injection training. Over 90% of patients learn to give themselves shots after one or two supervised sessions.

What Comes Next?
TNF inhibitors aren’t the only option anymore. IL-17 inhibitors like secukinumab and ixekizumab have shown similar effectiveness in head-to-head trials. But TNF blockers still dominate - they’re the most studied, the most proven, and the most widely used.
Future research is looking at smarter ways to pick who responds best - using gene profiles, gut microbiome data, and new biomarkers. There are also early trials for next-gen TNF inhibitors that target only the harmful receptor (TNFR1) while leaving the protective one (TNFR2) alone. That could mean fewer side effects.
For now, TNF inhibitors remain the gold standard. They don’t cure AS, but they give people their lives back. Many patients who once struggled to tie their shoes now hike, swim, or play with their kids without pain. That’s not just symptom control - it’s disease modification.
Starting TNF Inhibitor Therapy: What to Expect
If your doctor recommends a TNF inhibitor, here’s what happens next:
- **Screening**: Blood tests for TB, hepatitis B/C, and heart function.
- **Choice of drug**: Based on your lifestyle, insurance, and preferences (injection frequency, clinic visits).
- **Training**: For subcutaneous drugs, you’ll get a nurse to show you how to inject. Most people master it in one or two tries.
- **First dose**: Infliximab requires a clinic visit; others can be done at home.
- **Monitoring**: Blood tests every 3-6 months to check for inflammation and liver/kidney function.
- **Follow-up**: You’ll be assessed at 12 and 24 weeks using BASDAI and CRP to see if it’s working.
Don’t stop if you don’t feel better right away. It can take up to 3 months. And if one doesn’t work, don’t give up - switching is common and often successful.
Can TNF inhibitors stop spinal fusion in ankylosing spondylitis?
TNF inhibitors can slow or reduce radiographic progression - the process that leads to spinal fusion - especially if started early, within the first 2 years of symptoms. Studies show they cut progression by 50-60% in early AS. But they don’t stop it completely in everyone. Some bone growth still occurs over time, which is why combining medication with regular exercise and posture training is critical.
Do I have to stay on TNF inhibitors forever?
Most people stay on them long-term because stopping often leads to flare-ups. But some patients who achieve deep remission - with normal CRP, no pain, and no inflammation on MRI - may try to taper under close supervision. Only about 30% of those who try can stay off the drug without relapsing. For most, it’s a long-term treatment, like insulin for diabetes.
Are TNF inhibitors safe during pregnancy?
Yes, most TNF inhibitors are considered safe during pregnancy, especially adalimumab and etanercept. They cross the placenta less than other biologics. Many women continue treatment to keep AS under control - uncontrolled inflammation during pregnancy can lead to complications. Always discuss with your rheumatologist and OB-GYN before planning pregnancy.
What if TNF inhibitors don’t work for me?
About 30-40% of patients don’t respond well to the first TNF inhibitor. The next step is usually switching to another TNF blocker - and 30-40% of those patients respond. If that fails, IL-17 inhibitors like secukinumab or ixekizumab are the next best option. They work on a different pathway and can be very effective for people who didn’t respond to TNF blockers.
Can I use TNF inhibitors with NSAIDs or physical therapy?
Absolutely. TNF inhibitors work best when combined with NSAIDs for pain control and daily physical therapy for mobility. Exercise - especially swimming, yoga, and stretching - helps prevent stiffness and maintain posture. Medication alone isn’t enough. The combination is what keeps people mobile and independent long-term.
Final Thoughts
Ankylosing spondylitis doesn’t have to mean a life of pain and stiffness. TNF inhibitors have turned what was once a progressive, disabling disease into a manageable condition. They’re not perfect - they require injections, monitoring, and come with risks. But for the vast majority of patients, the benefits far outweigh the downsides.
If you’re living with AS and still struggling, talk to your rheumatologist about whether a TNF inhibitor could be right for you. Don’t wait until your spine starts fusing. Early treatment is the key to staying active, independent, and pain-free for decades to come.


Comments (15)