Every year, over 300,000 women die from cervical cancer - almost all of them from a preventable virus. The good news? We have the tools to stop it. HPV vaccination and regular Pap testing together have turned cervical cancer from a leading cause of death into one of the most preventable cancers on the planet. But only if people use them.
How HPV Causes Cervical Cancer
Almost all cases of cervical cancer are caused by the human papillomavirus, or HPV. It’s not just one strain - there are over 100 types, but only a few are dangerous. HPV types 16 and 18 are the worst, responsible for about 70% of all cervical cancers. The virus spreads through skin-to-skin contact during sex. Most people get it at some point in their lives, and their immune systems clear it without any symptoms. But for some, the infection sticks around. Over years, it can turn normal cells in the cervix into precancerous changes - and eventually, cancer.
The scary part? This process takes 10 to 20 years. That’s why catching it early makes all the difference. By the time symptoms show up - abnormal bleeding, pain during sex, pelvic pain - it’s often too late. Prevention isn’t about waiting for symptoms. It’s about stopping the virus before it starts.
How the HPV Vaccine Works
The HPV vaccine doesn’t treat infection. It prevents it. It trains your immune system to recognize and fight off the most dangerous strains before you’re ever exposed. Since the first vaccine was approved in 2006, the science has only gotten stronger. Today, the only HPV vaccine available in the U.S. is Gardasil-9. It protects against nine strains of HPV - including the two that cause 70% of cancers and five more that cause another 20%.
The vaccine is given as a shot in the arm. For kids starting before age 15, two doses are enough - six to twelve months apart. For those starting at 15 or older, three doses are needed. Over 98% of people who finish the full series develop strong, lasting antibodies. Studies show the vaccine is 97% effective at preventing cervical cancer when given before sexual activity begins.
Real-world results are staggering. In Scotland, where girls have been routinely vaccinated since 2008, a 2024 study found zero cases of invasive cervical cancer in over 138,000 women who received two doses at ages 12 to 13. In Sweden, girls vaccinated before age 17 saw an 88% drop in cervical cancer. In the U.S., cervical cancer deaths among young women have dropped 62% in the last decade - directly tied to rising vaccine use.
Who Should Get the Vaccine and When
The CDC and the American College of Obstetricians and Gynecologists (ACOG) recommend routine HPV vaccination at age 11 or 12. That’s not because kids are sexually active - it’s because their immune systems respond best at that age. The vaccine works best when given before any exposure to HPV. Catch-up vaccination is still effective through age 26. For adults 27 to 45, vaccination may still be helpful, especially if you haven’t been exposed to many HPV types. Talk to your doctor - it’s not one-size-fits-all.
Boys and men should also be vaccinated. HPV doesn’t just cause cervical cancer. It causes cancers of the throat, anus, penis, and mouth. Vaccinating boys helps protect future partners and reduces overall virus spread. In countries like Australia, where both boys and girls are vaccinated, high-grade cervical abnormalities have dropped by 85%.
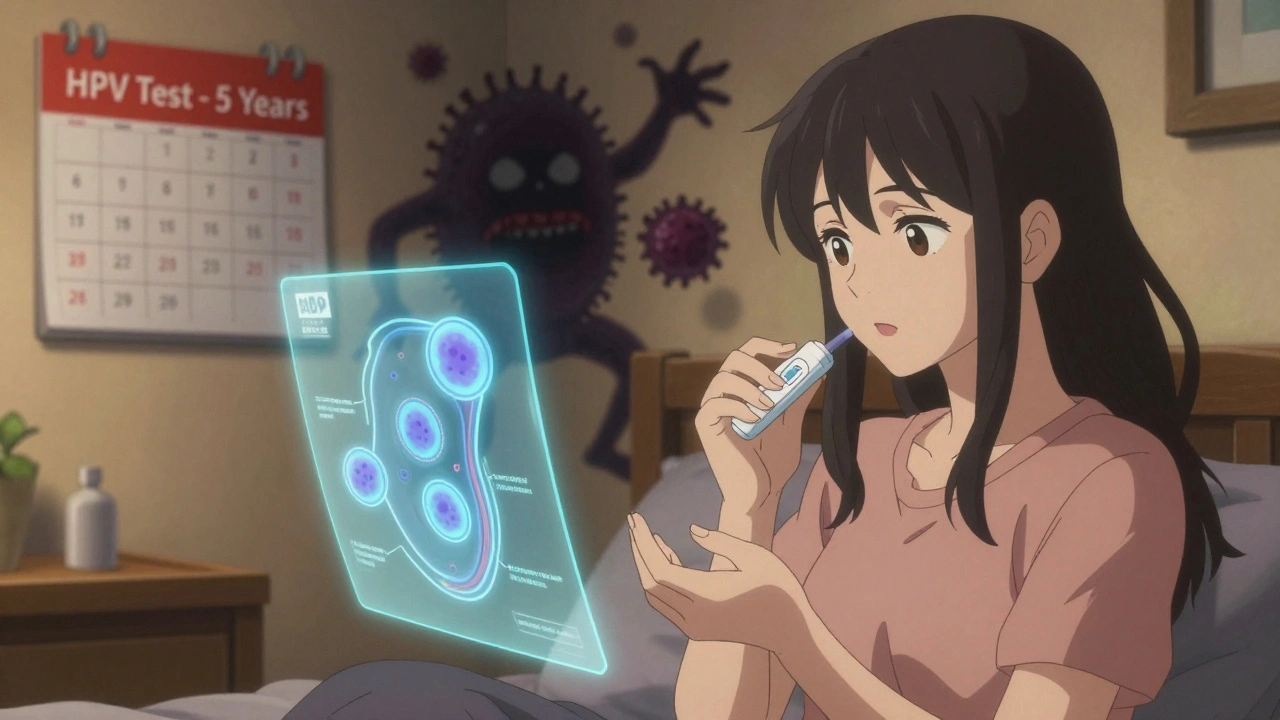
The Role of Pap Testing and HPV Screening
Even if you’ve been vaccinated, you still need screening. The vaccine doesn’t protect against every HPV strain, and some people were exposed before vaccination. That’s where Pap tests and HPV tests come in.
Pap tests - also called Pap smears - look for abnormal cells on the cervix. HPV tests look for the virus itself. Since 2023, ACOG and the CDC have updated guidelines: for most people, HPV testing alone every five years is the preferred method starting at age 25. If HPV is found, follow-up tests check for cell changes. If no HPV is found, you can wait five years before the next test.
Pap tests alone are still an option - every three years - but HPV testing is more accurate and catches problems earlier. For vaccinated women, screening intervals can be longer than for unvaccinated women. But no one gets a free pass. Vaccination and screening work together. One doesn’t replace the other.
What About Single-Dose Vaccines?
For years, the three-dose schedule was the norm. But new research is changing everything. A 2022 trial in Kenya found that just one dose of the HPV vaccine gave 97.5% protection against high-risk strains - and that protection lasted at least three years. A 2021 study in Costa Rica showed single-dose efficacy was nearly the same as two or three doses, even 11 years later.
This isn’t just science. It’s a lifeline for low-income countries. In places where getting three shots is hard because of cost, travel, or clinic access, one dose could mean the difference between prevention and tragedy. In 2023, the WHO prequalified single-dose HPV vaccines, and Gavi, the Vaccine Alliance, committed over $1 billion to roll them out in 50+ low-income countries.
The U.S. CDC now recognizes single-dose efficacy. While the official recommendation still says two or three doses depending on age, many clinics are starting to offer single-dose options for those who can’t return for follow-up shots. It’s not yet the standard, but it’s the future.

Why Vaccination Rates Are Still Too Low
Despite the science, only 60.4% of U.S. teens completed the HPV vaccine series in 2022. That’s far below the 80% target set by the CDC. Why? Misinformation. Fear. Lack of strong doctor recommendations. And the lingering myth that the vaccine encourages early sex - a claim completely debunked by multiple studies.
In rural areas, the problem is worse. While national cervical cancer rates have dropped, some rural counties are seeing rising cases. Access to clinics, lack of transportation, and fewer providers mean prevention isn’t reaching everyone. In contrast, countries like Australia and the UK have vaccination rates above 85%. Their success isn’t magic - it’s policy. School-based programs, automatic reminders, and public education made the difference.
What’s Next for Cervical Cancer Prevention
The goal isn’t just to reduce cervical cancer. It’s to eliminate it. The World Health Organization has set a 2030 target: 90% of girls vaccinated by 15, 70% of women screened by 35 and 45, and 90% of precancer cases treated. If we hit all three, we could cut cervical cancer cases by 95% by 2050.
New tools are helping. In January 2024, the FDA approved the first at-home HPV self-sampling test. Women can collect their own sample and mail it in. Early data shows this could increase screening rates by 40%, especially for those who avoid clinics due to embarrassment, fear, or access issues.
Experts agree: cervical cancer could become the first cancer to be eliminated - not just controlled, but gone - as a public health threat. But only if we act. Vaccinate early. Screen regularly. Push for access in your community. This isn’t just about medical science. It’s about choices - and the power to change outcomes.
What You Can Do Today
- If you’re 11-12, get your HPV vaccine on schedule - two doses, six months apart.
- If you’re 13-26 and haven’t been vaccinated, talk to your doctor. It’s not too late.
- If you’re 25 or older, get an HPV test every five years. Don’t wait for symptoms.
- If you’re a parent, don’t delay. Vaccinate your child before they turn 13.
- If you’re in a rural or underserved area, ask about mobile clinics or school-based programs.
One vaccine. One test. Two simple steps. Together, they can save your life - or the life of someone you love.
Is the HPV vaccine safe?
Yes. The HPV vaccine has been given to over 300 million people worldwide. Side effects are mild - sore arm, headache, or dizziness - and go away quickly. Serious reactions are extremely rare. It does not cause infertility, chronic pain, or neurological problems, as some rumors claim. The CDC, WHO, and every major medical group in the world agree: it’s safe.
Do I still need a Pap test if I got the HPV vaccine?
Yes. The vaccine protects against the most common cancer-causing strains, but not all of them. Screening catches the rest. Even if you’ve been vaccinated, you still need regular HPV testing starting at age 25. Skipping screening puts you at risk.
Can men get the HPV vaccine?
Yes. HPV causes cancers in men too - throat, anal, and penile cancers. The vaccine is approved for males up to age 26. It also helps protect future partners by reducing virus spread. Vaccinating boys is part of ending cervical cancer.
Is the HPV vaccine only for girls?
No. That’s an outdated idea. HPV affects everyone. The vaccine protects both men and women from multiple cancers. Countries that vaccinate both genders have seen faster declines in cervical and other HPV-related cancers. Gender-neutral vaccination is the new standard.
Can I get the HPV vaccine if I’m already sexually active?
Yes. Even if you’ve had sex, you may not have been exposed to all the HPV types the vaccine covers. It can still protect you from strains you haven’t encountered. The vaccine is recommended up to age 26 for everyone, regardless of sexual history.
What if I missed my second HPV shot?
Don’t restart. Just get the next dose as soon as you can. The CDC says you can wait up to a year between doses and still complete the series. The key is finishing - not timing. Even one dose offers strong protection, but two or three give the best long-term defense.
How often should I get screened after age 30?
If you’re 25-65, get an HPV test every five years. If you prefer, you can do co-testing (HPV plus Pap) every five years, or a Pap test alone every three years. HPV testing is more accurate and allows longer intervals. If your HPV test is negative, you’re at very low risk for the next five years.
Are at-home HPV tests reliable?
Yes. The FDA-approved at-home HPV test (like QIAsure) has been shown to be as accurate as clinic-based tests in clinical trials. It’s especially helpful for people who avoid exams due to fear, stigma, or lack of access. If you get a positive result, follow up with a provider - but the test itself works.
Can I get the HPV vaccine if I have HPV already?
Yes. The vaccine doesn’t treat existing infections, but it can protect you from other strains you haven’t caught yet. If you’ve had an abnormal Pap or HPV diagnosis, talk to your doctor. You may still benefit from vaccination, especially if you’re under 26.
Why isn’t the HPV vaccine mandatory in all states?
Vaccine requirements are decided by state governments, not the federal government. Some states require it for school entry, others don’t. But medical experts agree: it should be. Countries with mandatory school-based programs have near-universal coverage and are seeing cervical cancer disappear. The science is clear - the barrier is policy, not safety or effectiveness.





Comments (9)