Every year, thousands of people accidentally take two doses of the same medicine because they forgot whether they already took it. It’s not laziness or carelessness-it’s confusion. Maybe you were distracted. Maybe someone else gave the medicine and didn’t tell you. Or maybe your memory isn’t what it used to be. Whatever the reason, double-dosing is one of the most common-and dangerous-medication errors in homes across the UK and beyond.
Take paracetamol, for example. The maximum safe daily dose is 4,000mg. But if you’re taking a cold medicine that already contains paracetamol, and then you take a separate painkiller later, you could easily hit 5,000mg without realizing it. That’s enough to cause liver damage. Or consider blood thinners like warfarin: a single extra dose can lead to internal bleeding. These aren’t rare cases. In fact, nearly half of all medication-related emergencies happen at home, and double-dosing is a leading cause.
Why Double-Dosing Happens More Than You Think
It’s not just older adults. Parents, caregivers, people on multiple prescriptions, and even healthy adults who take vitamins or OTC meds are at risk. The problem grows when routines get disrupted-travel, holidays, hospital visits, or even daylight saving time changes. A 2023 study from Children’s Healthcare of Atlanta found that 41% of pediatric double-dosing incidents happened because one parent gave medicine after the child refused it, and another parent gave it again later without knowing.
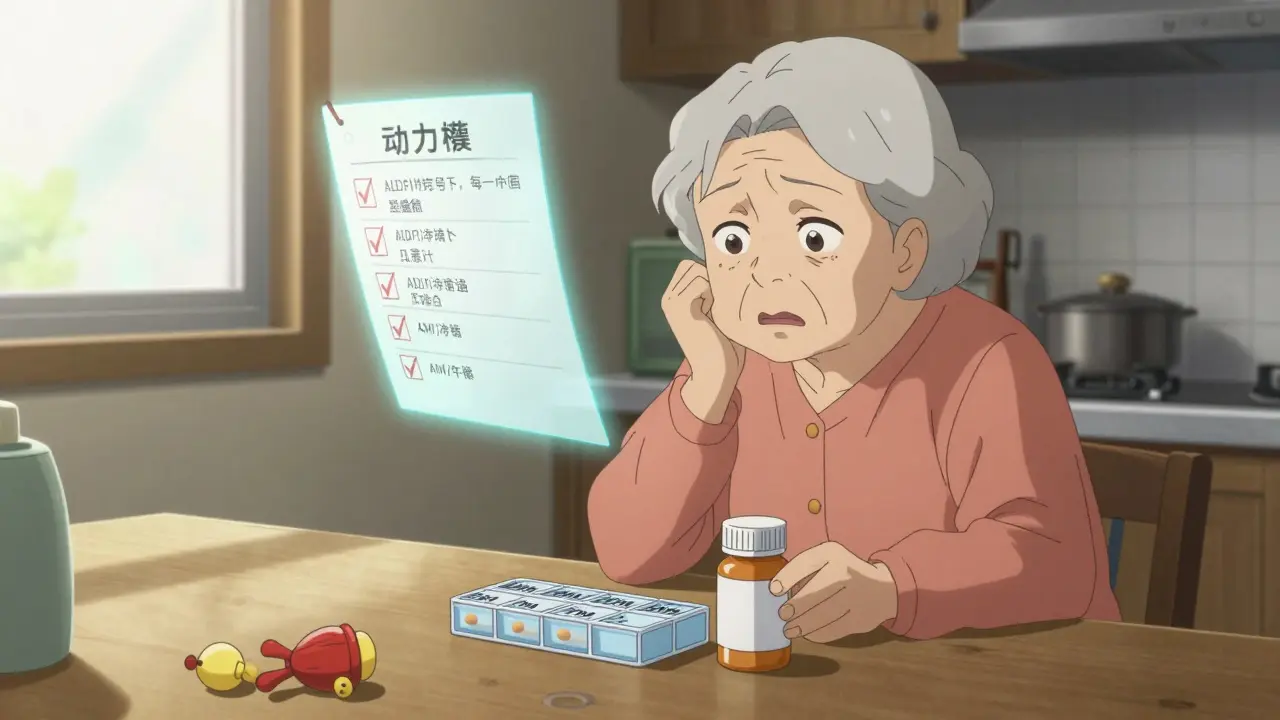
For seniors, the risk is even higher. The average person over 65 takes four to five prescription drugs daily. Add in supplements, painkillers, and sleep aids, and it’s easy to lose track. A survey by WesleyLife found that 63% of seniors worry weekly whether they’ve already taken their pills. And 28% admitted to double-dosing at least once in the past year.
Use a Pill Organizer-But Choose the Right One
One of the simplest, most proven tools is a pill organizer. Not just any organizer-get one with separate compartments for each time of day: morning, noon, evening, bedtime. A weekly version with four slots per day is ideal for most people on multiple medications.
Why does this work? Because you see it. If the compartment is empty, you know you’ve taken it. If it’s full, you haven’t. No guesswork. No mental tallying. St. Louis Children’s Hospital recommends this exact method because it’s visual, immediate, and doesn’t require technology.
And it’s effective. WesleyLife’s 2023 survey showed pill organizers reduced double-dosing by 35%. But when combined with another strategy-like a reminder system-the success rate jumps to 62%.
For older adults or those with memory issues, choose a large-print, easy-to-open model. Some even have alarms built in. Don’t be fooled by cheap plastic ones with flimsy lids-they often spill or get mislabeled. Stick to trusted brands sold through pharmacies or medical supply stores.
Set Digital Reminders-And Sync Them With Someone Else
Smartphones are powerful tools for medication safety. Apps like Medisafe, MyTherapy, or even the built-in calendar and alarms on your phone can send alerts at the exact time you need to take your medicine.
But here’s the key: don’t just set them for yourself. If you live with someone who helps manage your meds-your partner, adult child, or caregiver-share the reminders with them. That way, if you miss one, they’ll know. If you take one and forget to tell them, they’ll still get a notification and can check in.
A 2022 study in the Journal of Medical Internet Research found that users of medication reminder apps improved adherence by 87%. That’s not just about remembering-it’s about accountability. And when family members are involved in setting up the app, success rates rise even higher.
Never Use Kitchen Spoons to Measure Liquid Medicines
This one catches people off guard. If you’re giving liquid medicine to a child-or even taking it yourself-never use a kitchen teaspoon or tablespoon. They’re not accurate. A 2023 study by Children’s Healthcare of Atlanta found kitchen spoons vary in volume by 20% to 65%. That means what you think is 5mL could be 3mL or 8mL.
Always use the syringe, dropper, or cup that came with the medicine. If you lost it, ask your pharmacist for a new one. They’re free. And they’re calibrated to deliver the exact dose. For children, this isn’t just a suggestion-it’s a safety rule. Overdosing on liquid antibiotics or fever reducers can land a child in the ER.

Keep a Master Medication List
Write down every single thing you take: prescriptions, over-the-counter drugs, vitamins, herbal supplements, even eye drops or topical creams. Include the name, dose, and reason you’re taking it. Update it every time your doctor changes something.
Why? Because many double-dosing cases happen when two different medicines contain the same active ingredient. For example, many cold medicines contain acetaminophen. So do some painkillers. If you’re taking both, you’re doubling up without knowing it. EssexCare Pharmacy found that 32% of double-dosing incidents they reviewed in 2023 involved hidden duplicate ingredients.
Bring this list to every doctor’s appointment. Show it to your pharmacist when you pick up a new prescription. It’s your best defense against accidental overlap.
Assign One Person to Handle Medications
In households with multiple caregivers-especially with children or elderly relatives-confusion is inevitable. One person gives the medicine in the morning. Another gives it at lunch because they didn’t know it was already given. It happens more than you think.
St. Louis Children’s Hospital and other experts recommend designating one person as the official medication giver. That doesn’t mean they do it alone forever-it means they’re the one who tracks it, communicates it, and makes sure no one else gives a dose without checking in first.
This simple change reduced double-dosing incidents by 47% in homes studied by the hospital. For families, it’s not about control-it’s about clarity.
Store Medicines Out of Reach and Out of Sight
Most pediatric overdoses happen because kids find medicine that’s left out. Not just on counters-on nightstands, in purses, in coat pockets. A 2023 report from Children’s Healthcare of Atlanta showed that 86% of ER visits for medicine poisoning in children involved pills or liquids taken from a family member’s belongings.
Keep all medicines-yours and theirs-in a locked cabinet, high up, away from kids and pets. Even if you think your child “wouldn’t reach it,” they will. And don’t assume a child-proof cap is enough. They’re designed to slow down toddlers, not stop determined ones.

Use Simple Visual Cues for Single Daily Doses
If you only take one pill a day, a pill organizer might be overkill. In that case, try the bottle-flip method. After you take your dose, turn the bottle upside down. When you next see it, if it’s still upside down, you’ve taken it. If it’s upright, you haven’t.
Stanford Medicine tested this against pillboxes and found it worked better for single-dose regimens because it’s immediate and doesn’t require extra tools. It’s low-tech, free, and hard to forget.
What to Do If You Accidentally Double-Dose
If you realize you’ve taken two doses, don’t panic-but don’t wait either. Call 1-800-222-1222 immediately. That’s the Poison Help line in the US, and it’s free, confidential, and staffed 24/7 by poison control experts. In the UK, call NHS 111 and ask for the poison control team.
Have the medicine bottle handy. Tell them the name of the drug, how much you took, when you took it, and your age or your child’s age. They’ll tell you whether to wait, monitor symptoms, or go to the hospital.
Don’t try to induce vomiting unless they tell you to. Don’t give milk or charcoal unless instructed. Just call. The sooner you get expert advice, the safer you’ll be.
Future Tools Are Coming-But Simplicity Still Wins
Smart pill dispensers that lock after each dose are becoming more common. Johns Hopkins found they cut double-dosing by 76%. AI apps that learn your routine and warn you when you’re about to take a duplicate are on the horizon too.
But here’s the truth: the most effective tools today are still the simplest. A pill organizer. A reminder on your phone. A written list. A designated person. A locked cabinet.
You don’t need fancy gadgets. You need consistency, communication, and clarity. The technology helps-but the human habits keep you safe.
Start Today-One Step at a Time
You don’t have to fix everything at once. Pick one thing to change this week:
- Buy a weekly pill organizer with AM/PM slots.
- Set a daily phone reminder with a shared contact.
- Write down every medication you take-including supplements.
- Move all medicines to a locked cabinet.
- Assign one person to be the medication tracker.
Do one. Then do another next week. Medication safety isn’t about perfection-it’s about reducing risk, one small step at a time.
What should I do if I’m not sure whether I took my medicine?
If you’re unsure, don’t guess. Check your pill organizer, your medication log, or your phone reminder. If you still can’t tell, skip the dose and wait until the next scheduled time. Taking an extra dose can be dangerous. Never double up to make up for a missed one unless your doctor says so.
Can over-the-counter medicines cause double-dosing?
Yes, absolutely. Many cold, flu, and pain relief products contain the same active ingredients as prescription drugs-like acetaminophen, ibuprofen, or diphenhydramine. Always check the ‘Active Ingredients’ label on OTC boxes. If it matches your prescription, you’re at risk of doubling up. Keep a master list of everything you take, including vitamins and herbal supplements.
Is it safe to split pills to save money?
Only if your doctor or pharmacist says it’s okay. Some pills are designed to release medicine slowly and shouldn’t be split. Others have coatings that protect your stomach or control absorption. Splitting them can change how they work. Always ask before cutting any pill-even if it looks easy to break.
How often should I update my medication list?
Update it every time you start, stop, or change a medication-including doses. Do this after every doctor’s visit, pharmacy refill, or hospital discharge. Keep a printed copy in your wallet and a digital version on your phone. Share it with your main caregiver and your pharmacist.
Are pill organizers only for seniors?
No. Anyone taking more than one medication a day can benefit-from people with diabetes and high blood pressure to those managing mental health meds or chronic pain. Even young adults on birth control and antibiotics can use them to avoid missed or double doses. It’s not about age-it’s about complexity.
What if I forget to take my medicine at the right time?
If you miss a dose, check the instructions on the label or ask your pharmacist. For most medications, if it’s been less than half the time until your next dose, take it as soon as you remember. If it’s close to the next dose, skip it. Never take two doses at once unless instructed. Setting a daily reminder and linking your dose to a routine (like brushing teeth) helps prevent missed doses.
Can I rely on my memory to remember my meds?
No. Memory is unreliable, especially under stress, fatigue, or when taking multiple medications. Even people with sharp memories make mistakes. Studies show that people who rely only on memory are twice as likely to double-dose compared to those who use visual or digital tools. Use a system-don’t trust your brain alone.
Do I need a smartphone to use digital reminders?
Not necessarily. Many basic phones have alarm functions. You can also use a dedicated medication alarm clock, which doesn’t require internet or apps. Some pharmacies offer free pill dispensers with built-in alarms. The goal isn’t to use the fanciest tech-it’s to find a system you’ll actually use every day.


Comments (12)