Oral Thrush Risk Calculator
Assess Your Risk
Answer these questions to see your risk of oral thrush or hoarseness from inhaled corticosteroids. The more factors you have, the higher your risk.
Tip: You can reduce your risk by 60-80% by rinsing and using a spacer correctly. Learn more in the article.
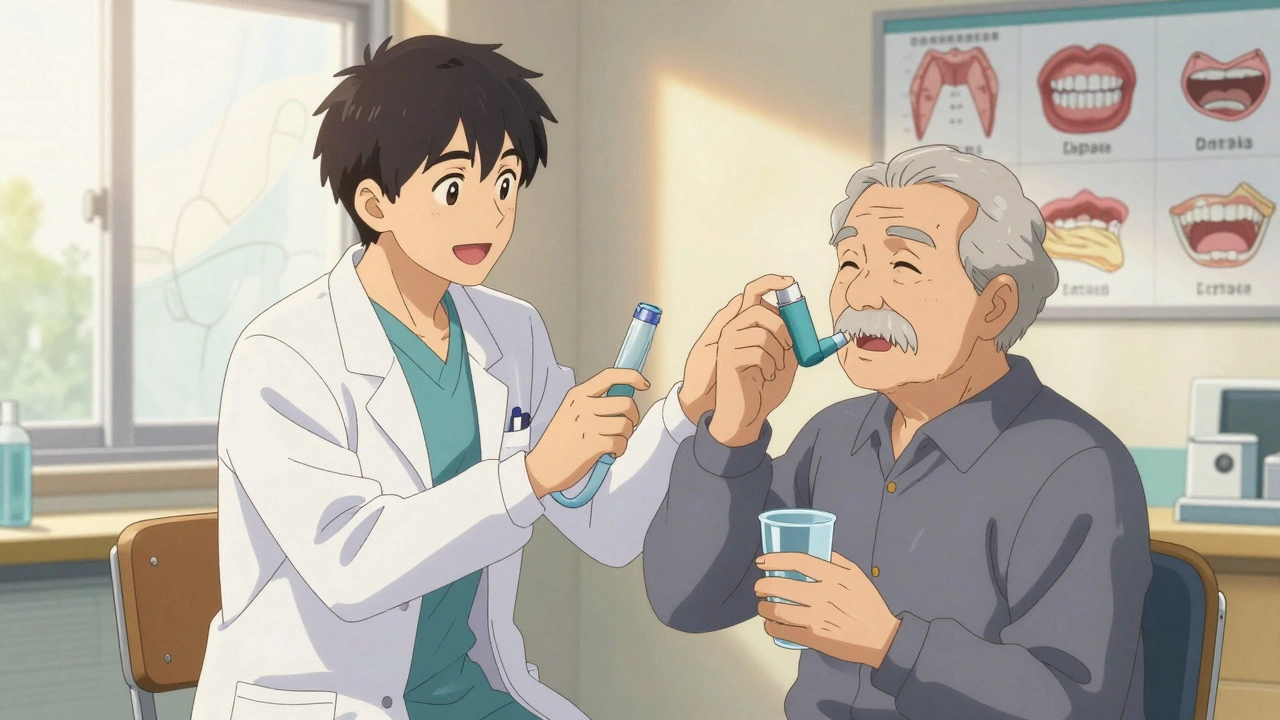
When you use an inhaled corticosteroid for asthma or COPD, you’re doing exactly what your doctor asked: reducing lung inflammation, preventing attacks, and breathing easier. But if you don’t take a few simple steps after each puff, you could end up with white patches in your mouth, a burning tongue, or a voice that sounds like gravel. These aren’t rare side effects-they’re common, preventable, and often ignored.
Why Your Inhaler Is Causing Oral Thrush
Inhaled corticosteroids like fluticasone (Flovent), budesonide (Pulmicort), and beclomethasone (Qvar) are designed to target your airways. But here’s the problem: up to 80% of the medication doesn’t make it to your lungs. Instead, it sticks to the back of your throat and your tongue. That’s not a flaw in the device-it’s how inhalers work. When corticosteroids sit in your mouth, they dampen your local immune response. Normally, your mouth has harmless yeast called Candida albicans living in it. But when the immune system is suppressed by the steroid, that yeast overgrows. The result? Oral thrush: creamy white patches on your tongue, inner cheeks, or throat. They might look like milk curds. If you scrape them off, you’ll see red, raw skin underneath. It can hurt to swallow, make food taste strange, or even cause a burning sensation. This isn’t just about discomfort. For people with diabetes, older adults, or those on high doses of steroids, thrush can become a recurring problem. And if left unchecked, it can spread to your esophagus, making swallowing painful and even dangerous.Why Your Voice Is Sounding Hoarse
Hoarseness is another side effect you might not connect to your inhaler. But it’s direct: steroid particles landing on your vocal cords cause swelling and irritation. You might notice your voice cracks, sounds raspy, or disappears entirely after using your inhaler. It usually clears up in a few hours, but if you’re using your inhaler multiple times a day, that hoarseness can become a daily annoyance. Some people stop using their inhaler because of this. That’s dangerous. Uncontrolled asthma leads to more hospital visits, missed work, and long-term lung damage. The answer isn’t to skip doses-it’s to change how you use the inhaler.The Two Best Ways to Prevent Both Problems
There are two proven, simple strategies that cut the risk of thrush and hoarseness by 60-80%. They’re not new. They’re not expensive. But most people don’t do them right-or at all. 1. Rinse, gargle, swish, and spit after every use. This isn’t just “rinse your mouth.” You need to be thorough. After you inhale, take a sip of water, swish it around your mouth for 15-20 seconds, then gargle deeply in the back of your throat. Spit it out. Don’t swallow it. Do this every single time-even at night, even if you’re tired, even if you’re using a spacer. Studies show that people who do this consistently reduce their chance of thrush by 60-70%. One patient on an asthma forum said: “I got thrush twice before I started rinsing properly. Now I do it every time. No more white patches in five years.” 2. Use a spacer with your metered-dose inhaler (MDI). If you’re using a traditional puff inhaler (not a dry powder device), a spacer is non-negotiable. A spacer is a plastic tube that attaches to your inhaler. It holds the medicine in a chamber so you can breathe it in slowly. Without it, large particles crash into your throat. With it, only the fine particles that reach your lungs stay airborne. Research shows that using a spacer reduces oral deposition by up to 50%. That means less steroid sitting on your tongue and vocal cords. You don’t need a fancy one. A simple, clean plastic spacer from your pharmacy works fine.
What About Dry Powder Inhalers?
Dry powder inhalers (DPIs) like Asmanex or Pulmicort Flexhaler don’t require a spacer because they deliver medication as a fine powder you inhale quickly. But they’re not risk-free. You still get residue in your mouth. The same rinsing rule applies. Skip it, and you’re still at risk. Some people think, “I use a DPI, so I don’t need to rinse.” That’s a myth. The 2025 review in Healthcare (Basel) clearly states: “Mouth rinsing after inhalation remains essential regardless of inhaler type.”What If You Already Have Thrush?
If you see white patches, feel pain, or lose your taste, don’t wait. See your doctor. Oral thrush is treated with antifungal medications like nystatin oral suspension (a liquid you swish and swallow) or clotrimazole lozenges. Treatment usually takes 7-14 days. But here’s the catch: if you don’t fix your inhaler technique, thrush will come back. Medication treats the infection. Proper rinsing and spacer use prevent it.Other Things That Make It Worse
Some habits increase your risk more than others:- High doses: Using more than 800 mcg per day of beclomethasone equivalent (or equivalent doses of other steroids) raises your risk significantly.
- Diabetes: High blood sugar feeds Candida. If your HbA1c is above 7.0%, you’re at higher risk.
- Dry mouth: Medications for blood pressure, depression, or allergies can reduce saliva. Less saliva means less natural cleaning of your mouth.
- Poor dental hygiene: Not brushing or flossing regularly lets yeast and bacteria build up.
- Not cleaning your spacer: If your spacer gets gunky with leftover medicine, it becomes a breeding ground for fungus. Wash it weekly with mild soap and let it air dry.
What You’re Probably Doing Wrong
Most people think they’re doing enough. They rinse quickly. They use a spacer but forget to shake it out. They skip rinsing after nighttime doses. Here’s what the data shows:- Only 45% of patients rinse after every use, according to a 2023 European study.
- 65% of patients forget to rinse after their nighttime inhaler.
- One in three patients don’t clean their spacer at all.
What’s New in 2025
Newer inhalers are being designed to reduce throat deposition. Some now have built-in spacers. Others use different drug formulations that stick less to oral tissue. But these are still in early adoption. The biggest change isn’t in the device-it’s in the care model. More clinics are now pairing respiratory therapists with dental professionals. One pilot program in the U.S. showed a 35% drop in oral thrush cases when patients got both asthma education and a dental check-up every six months. And there’s emerging research on probiotic mouthwashes. Some small studies suggest that rinsing with a probiotic solution (like those containing Lactobacillus) may help crowd out Candida. But this isn’t standard yet. Stick to water for now.Real Talk: It’s Not Just About Health-It’s About Trust
Many patients stop using their inhalers because they’re scared of side effects. They hear “steroid” and think “weight gain,” “bone loss,” or “thrush.” But the truth is: the risks of not using your inhaler are far worse than the side effects. The side effects are manageable. The disease isn’t. Rinsing after your inhaler takes 30 seconds. It costs nothing. It doesn’t interfere with your medication. It’s the single most effective thing you can do to protect your mouth and your voice. If you’ve had thrush before, you know how annoying it is. If your voice has been hoarse for months, you know how frustrating it is to sound like you’re sick every day. Don’t wait until it happens again. Start today. Rinse. Gargle. Spit. Use your spacer. Clean it once a week. That’s it. Your lungs will thank you. So will your throat.Can I just rinse with mouthwash instead of water?
It’s better to use plain water. Alcohol-based mouthwashes can dry out your mouth, which makes thrush more likely. Some mouthwashes contain sugars or artificial sweeteners that can feed yeast. Water is the safest, most effective choice. If you want to use mouthwash, do it at least an hour after rinsing with water-never right after your inhaler.
Do I need to rinse if I use a dry powder inhaler?
Yes. Dry powder inhalers still leave residue in your mouth and throat. Even though they don’t require a spacer, you’re still exposing your oral tissues to the steroid. Rinsing after each use reduces your risk of thrush and hoarseness. Don’t skip it just because the device feels different.
Is oral thrush contagious from my inhaler?
No. Oral thrush isn’t spread from person to person through inhalers. The yeast that causes it (Candida albicans) is already in your mouth. It’s your own immune system that lets it overgrow when steroids suppress it. But sharing inhalers or spacers is still a bad idea-because you could transfer bacteria or viruses.
Can I brush my teeth right after using my inhaler?
Yes, and it’s actually a good idea. Brushing your teeth after rinsing helps remove any remaining particles and stimulates saliva flow. Just wait at least 15 minutes after rinsing to avoid scrubbing away protective enamel that may be softened by the steroid. Use a soft-bristled brush and fluoride toothpaste.
How often should I clean my spacer?
Once a week. Wash it with warm water and a drop of mild dish soap. Don’t scrub the inside too hard-you don’t need to remove every trace of medicine, just enough to prevent buildup. Let it air dry completely before using it again. A dirty spacer can harbor fungus and bacteria, which defeats the purpose of using it.
Will using a spacer make my inhaler less effective?
No. In fact, it makes your inhaler more effective. Spacers help more medicine reach your lungs because you breathe in slowly and deeply. Without a spacer, a lot of the dose hits your throat and gets swallowed or stuck. Studies show that using a spacer improves lung delivery by 30-50% and cuts side effects by the same amount.
I’m on a high dose of steroids. Can I still avoid thrush?
Yes, but you need to be extra careful. High-dose users should always use a spacer, rinse and gargle after every puff, and brush their teeth twice daily. Consider asking your doctor if switching to a lower-dose combination inhaler (like one with a long-acting bronchodilator) is possible. Also, monitor your mouth weekly for early signs of white patches. Catching it early means faster treatment.



Comments (10)