When your doctor puts Isordil (Isosorbide Dinitrate) on the prescription pad, you might wonder if there’s a better fit for your chest pain or heart‑failure regimen. The truth is, the world of vasodilators is crowded, and each option brings its own rhythm of onset, duration, and side‑effect profile. Below we break down the most common alternatives, line them up side‑by‑side, and give you a “what‑works‑for‑me” cheat sheet you can use at the next appointment.
What Is Isordil and How Does It Work?
Isordil belongs to the organic nitrate family. After you swallow a tablet, the drug releases nitric oxide (NO) inside the smooth muscle lining of blood vessels. NO triggers a cascade that relaxes the muscle, widening (dilating) arteries and veins. The result is lower cardiac workload and reduced oxygen demand, which eases angina and can improve symptoms in certain types of heart failure.
Key attributes of Isordil:
- Class: Organic nitrate
- Typical uses: Chronic angina prophylaxis, acute decompensated heart failure (as adjunct)
- Onset: 30‑45 minutes
- Duration: 6‑8 hours (once‑daily dosing for maintenance)
- Common side effects: Headache, dizziness, flushing, hypotension
Why Look at Alternatives?
Even though Isordil is effective, real‑world patients hit a few snags:
- Tolerance - Repeated exposure can blunt the vasodilatory response, forcing doctors to add a nitrate‑free interval.
- Unpleasant headaches that can interfere with work or sleep.
- Interaction concerns with phosphodiesterase‑5 inhibitors (e.g., Viagra) or certain antibiotics.
- Convenience - some people prefer a patch or a sublingual tablet over a pill they must take at the same time every day.
If any of these ring a bell, it’s worth exploring the alternatives listed below.
Top Alternatives to Isordil
We’ve grouped the alternatives into three buckets: other nitrates, long‑acting nitrate monotherapy, and non‑nitrate vasodilators. Each entry includes a quick definition (microdata appears on first mention) and the pros/cons you’ll hear most often.
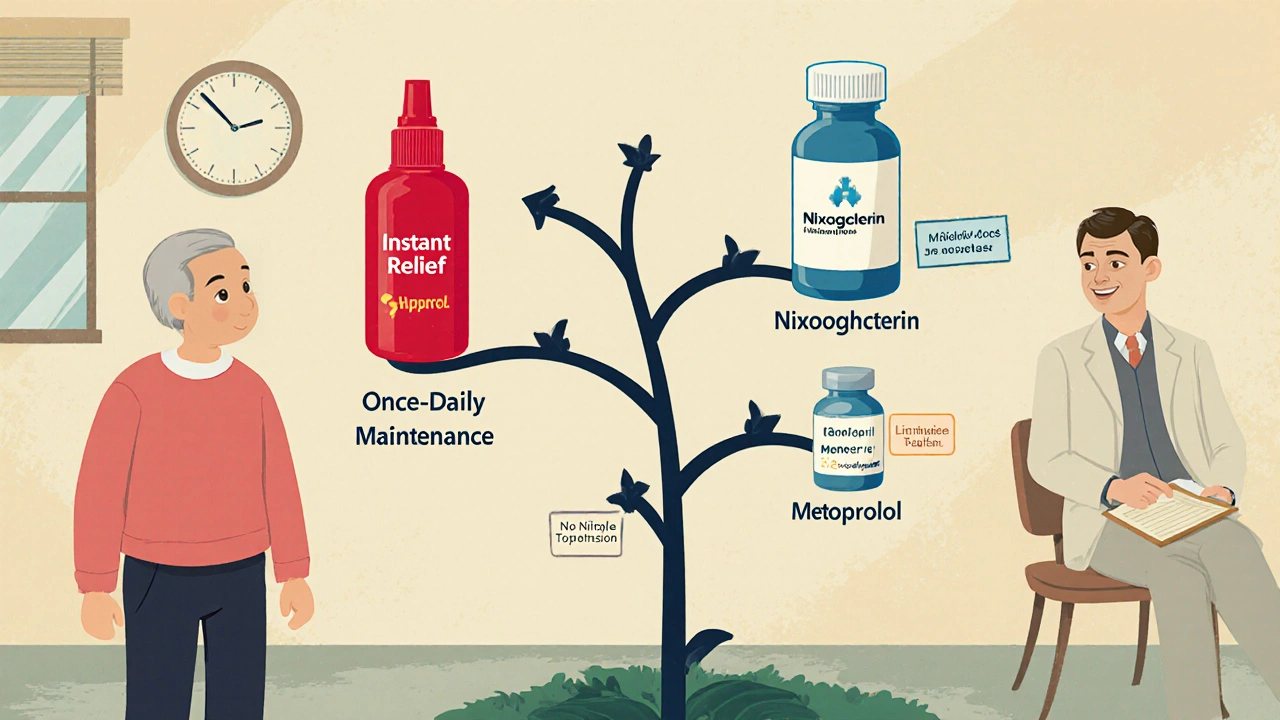
Nitroglycerin (glyceryl trinitrate, GTN) is the classic “fast‑acting” nitrate. It comes in sublingual tablets, sprays, and transdermal patches. Onset can be as quick as 1‑2 minutes, making it ideal for acute angina attacks.
- Pros: Immediate relief, multiple dosage forms.
- Cons: Short duration (15‑30min), requires strict storage away from light and heat.
Isosorbide Mononitrate (often sold as Imdur) is the single‑dose cousin of Isordil. It provides a smoother, longer‑lasting effect without the need for a nitrate‑free window.
- Pros: Once‑daily dosing, less headache than Isordil for many patients.
- Cons: Still a nitrate, so tolerance can develop over weeks.
Hydralazine is a direct‑acting arteriolar vasodilator. It’s not a nitrate, so it circumvents nitrate tolerance and can be combined with nitrates for synergistic effect.
- Pros: Works on resistant hypertension, useful in combination therapy for heart failure.
- Cons: Can cause reflex tachycardia and a lupus‑like syndrome with long‑term use.
Lisinopril (Prinivil) represents the ACE‑inhibitor class. Though not a pure vasodilator, it reduces afterload by inhibiting angiotensin‑II, making it a solid alternative for patients who can’t tolerate nitrates.
- Pros: Proven mortality benefit in heart failure, once‑daily dosing.
- Cons: Cough in up to 10% of users, contraindicated in pregnancy.
Metoprolol is a beta‑blocker that reduces heart rate and contractility, cutting myocardial oxygen demand. It’s often prescribed when angina persists despite nitrate therapy.
- Pros: Controls arrhythmias, improves survival post‑myocardial infarction.
- Cons: Can exacerbate asthma, may cause fatigue or depression.
Side‑by‑Side Comparison Table
| Drug | Class | Typical Use | Onset | Duration | Common Side Effects | Typical UK Cost (per month) |
|---|---|---|---|---|---|---|
| Isordil (Isosorbide Dinitrate) | Organic nitrate | Chronic angina prophylaxis, adjunct heart failure | 30‑45min | 6‑8h | Headache, flushing, hypotension | ≈£8‑£12 |
| Nitroglycerin | Organic nitrate | Acute angina relief | 1‑2min | 15‑30min | Severe headache, hypotension, dizziness | ≈£5‑£9 (tablet/spray) |
| Isosorbide Mononitrate | Organic nitrate (single dose) | Chronic angina, heart failure | 45‑60min | 12‑24h | Mild headache, nausea | ≈£10‑£14 |
| Hydralazine | Direct arteriolar vasodilator | Resistant hypertension, heart failure (combo) | 15‑30min | 4‑6h | Tachycardia, lupus‑like rash | ≈£6‑£10 |
| Lisinopril | ACE inhibitor | Heart failure, hypertension | 1‑2h | 24h | Cough, hyperkalaemia, dizziness | ≈£4‑£8 |
| Metoprolol | Beta‑blocker | Angina, post‑MI, heart failure | 30‑60min | 12‑24h | Fatigue, bradycardia, sexual dysfunction | ≈£5‑£9 |
How to Choose the Right Option for You
Picking a medication isn’t a one‑size‑fits‑all decision. Below is a quick decision tree you can run through during your next doctor’s visit:
- If you need instant relief for sudden chest pain, the answer is almost always nitroglycerin.
- If you’re looking for once‑daily maintenance with fewer headaches, try isosorbide mononitrate.
- If you’ve hit nitrate tolerance despite a nitrate‑free interval, consider switching to a non‑nitrate such as lisinopril or hydralazine.
- If you have co‑existing hypertension or heart failure, a combination (e.g., hydralazine + nitrates) may give better control.
- If you’re on erectile‑dysfunction medication, avoid any organic nitrate - ACE inhibitors or beta‑blockers are safer.
The key is open communication: tell your clinician about every over‑the‑counter product, supplement, and lifestyle habit that could interact.
Practical Tips to Minimize Side Effects
- Start low, go slow: Begin with the smallest dose that relieves symptoms, then titrate upward.
- Hydration matters: Keeping a bottle of water handy can blunt sudden drops in blood pressure.
- Headache hack: A low‑dose aspirin (if not contraindicated) taken 30minutes before your nitrate can reduce the throbbing.
- Nitrate‑free interval: Even with once‑daily dosing, leave a 10‑hour window without the drug to reset tolerance.
- Storage tip: Store all nitrate tablets in a cool, dark place; moisture can degrade potency.
When to Seek Immediate Care
Even the best medication won’t help if you ignore warning signs. Call emergency services (999 in the UK) if you experience:
- Chest pain that lasts longer than 5minutes despite taking your rescue medication.
- Sudden severe shortness of breath, fainting, or palpitations.
- Signs of a serious allergic reaction - swelling of lips or throat, rash, difficulty breathing.
These symptoms suggest a cardiac event that needs fast hospital treatment, not just a dose adjustment.
Bottom Line Checklist
- Identify whether you need acute or maintenance therapy.
- Match onset/duration to your daily routine (quick‑acting vs long‑acting).
- Check for drug interactions (especially with PDE‑5 inhibitors).
- Discuss tolerance‑prevention strategies with your prescriber.
- Monitor side effects and keep a symptom diary for the first 2‑3 weeks.
Frequently Asked Questions
Can I take Isordil and nitroglycerin together?
Usually no. Combining two organic nitrates can cause severe hypotension and intense headaches. Doctors may prescribe a nitrate‑free interval and use nitroglycerin only as a rescue pill, but they will adjust the dosing schedule carefully.
Why do I get a headache after taking Isordil?
The headache comes from rapid dilation of blood vessels in the brain, a direct effect of nitric oxide. It’s a common side effect of all nitrates. If it’s mild, spacing the dose or taking a low‑dose aspirin beforehand often helps.
Is isosorbide mononitrate safer than Isordil?
Safety profiles are similar because both are nitrates. However, isosorbide mononitrate delivers a steadier plasma level, so many patients report fewer breakthrough headaches. It also eliminates the need for a nitrate‑free interval, which can simplify dosing.
Can I replace Isordil with an ACE inhibitor?
ACE inhibitors work differently - they lower blood pressure by blocking angiotensin‑II, not by dilating veins directly. They are excellent for heart‑failure patients, but they may not relieve angina as quickly as nitrates. Some clinicians use a combo approach, starting with an ACE inhibitor and adding a nitrate if chest pain persists.
What should I do if I miss a dose of Isordil?
Take the missed dose as soon as you remember, unless it’s within 4hours of the next scheduled dose. In that case, skip the missed one and resume your regular schedule to avoid double‑dosing and excessive blood‑pressure drop.
By weighing onset time, duration, side‑effect risk, and cost, you can zero in on the medication that fits your lifestyle and medical needs. Talk to your heart specialist armed with this comparison, and you’ll walk away with a clear, personalized plan.


Comments (11)