When you hear that hepatitis C has been cured, it’s natural to think the danger is over. After all, the virus is gone. Blood tests show no trace of it. You feel better. But here’s the hard truth: liver cancer risk after SVR doesn’t vanish-even when the virus is completely cleared. If you had advanced liver scarring before treatment, your risk of liver cancer remains real. And skipping follow-up scans could cost you your life.
What SVR Really Means-and What It Doesn’t
Sustained Virologic Response, or SVR, means the hepatitis C virus is undetectable in your blood 12 or 24 weeks after finishing treatment. With today’s direct-acting antivirals (DAAs), over 95% of people achieve this. It’s a medical win. But SVR isn’t a clean slate for your liver. It’s a new starting point.
Studies show SVR cuts liver cancer risk by about 71%. That sounds impressive-and it is. But that still leaves nearly 3 out of 10 people with some level of ongoing risk. And that risk isn’t spread evenly. It’s concentrated in people who already had cirrhosis or advanced fibrosis before treatment.
Think of it like quitting smoking. Your lung cancer risk drops sharply, but if you smoked for 30 years, your risk never goes back to that of someone who never smoked. The same applies here. The liver doesn’t magically reset. Damage from years of inflammation doesn’t disappear overnight.
The Real Culprit: Fibrosis, Not the Virus
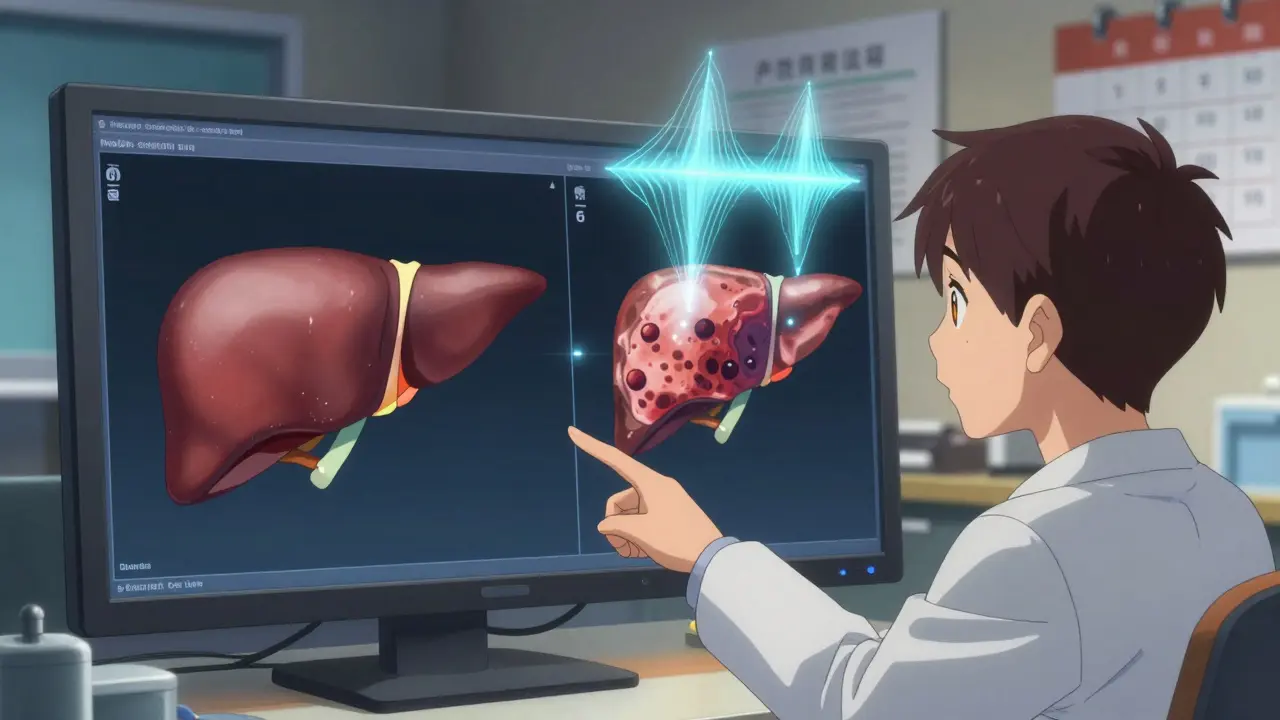
The biggest predictor of liver cancer after SVR isn’t the virus-it’s the scar tissue. That’s fibrosis. When the liver is damaged repeatedly by hepatitis C, it tries to heal by forming fibrous bands. Over time, this turns into cirrhosis: a hardened, knotted liver that can’t function properly.
Even after the virus is gone, those scars remain. And scarred tissue is more likely to turn cancerous. Research shows that patients with F3 fibrosis (advanced) or F4 (cirrhosis) before treatment have a persistent risk of developing hepatocellular carcinoma (HCC)-the most common form of liver cancer.
Here’s what the numbers say:
- People with cirrhosis who achieved SVR still develop liver cancer at a rate of about 2.1 to 2.3 per 100 person-years.
- That’s less than half the rate of untreated cirrhotic patients (4.5 per 100 person-years), but it’s still high enough to warrant action.
- Patients without advanced fibrosis before treatment? Their risk is extremely low-so low that most experts don’t recommend ongoing screening for them.
The key is knowing where you stood before treatment. If your liver biopsy, FibroScan, or FIB-4 score showed advanced scarring, you’re in the high-risk group. No matter how good you feel, you need regular check-ups.
Who Needs Surveillance-and Who Doesn’t
There’s a major split in global guidelines. In Europe, the recommendation is clear: if you had F3 or F4 fibrosis before treatment, get an ultrasound every six months-forever. In the U.S., the American Association for the Study of Liver Diseases (AASLD) says only those with cirrhosis (F4) need ongoing screening. They don’t recommend it for F3 patients.
Why the difference?
European experts worry that fibrosis can be misclassified. A liver scan might show F3, but in reality, it’s early cirrhosis. And once cancer develops, it’s too late. They argue: it’s cheaper and safer to screen everyone with advanced scarring than to miss one case.
U.S. experts counter that F3 patients often see fibrosis improve after SVR. Their cancer risk drops so low that screening may do more harm than good-false positives lead to unnecessary biopsies, anxiety, and costs.
Here’s what most doctors agree on:
- If you had cirrhosis before treatment → keep getting screened every 6 months.
- If you had advanced fibrosis (F3) and your liver has improved since SVR → discuss whether screening can be extended to once a year.
- If you had minimal or no fibrosis → no routine screening needed.
Tools like FibroScan (transient elastography) and FIB-4 scores help track changes. If your FibroScan reading drops below 9.5 kPa after SVR, your risk may be low enough to consider longer intervals between scans.
The Screening Gap: Why Most People Skip It
Even when guidelines exist, people don’t follow them. A 2023 study found that only about 25% of eligible patients get the recommended ultrasound screenings after SVR.
Why?
- Patients think they’re cured-so they stop going to the doctor.
- Doctors assume the patient knows they need follow-up and don’t emphasize it.
- Access to ultrasound machines is limited in rural areas.
- There’s no standard way to track who needs screening after treatment.
One big problem: patients are rarely told that their cancer risk didn’t disappear. They’re told, “You’re cured.” And they believe it. That’s dangerous.
Health systems are starting to fix this. The U.S. Veterans Health Administration added automated reminders to their electronic records. After the change, post-SVR screening rates jumped by 32%. Simple nudges work.
What You Should Do Now
If you’ve achieved SVR, here’s what to do:
- Find out your fibrosis stage before treatment. Check your medical records for FibroScan, FIB-4, or liver biopsy results.
- If you had F3 or F4 → schedule a liver ultrasound every six months. Ask if your doctor also checks alpha-fetoprotein (AFP), though ultrasound alone is usually enough.
- If you had F0-F2 → you likely don’t need routine screening. But if you have other risk factors (alcohol use, obesity, diabetes), talk to your doctor.
- Get a FibroScan or FIB-4 test 6-12 months after SVR. If your score improved significantly, your risk may be dropping. This could mean longer intervals between scans.
- Don’t assume you’re off the hook. Even if you feel great, your liver still needs monitoring.
There’s no magic pill that erases past damage. But catching liver cancer early-when it’s still small and treatable-can mean the difference between survival and death. Surveillance isn’t about fear. It’s about control.

The Future: Personalized Surveillance
One-size-fits-all screening is outdated. Researchers are now building dynamic models that adjust based on how your liver changes over time.
At Massachusetts General Hospital, a new calculator uses serial FibroScan results to predict risk. Early data shows that 42% of F3 patients with stable or improving fibrosis after SVR could safely switch to yearly scans instead of every six months.
Other tools are on the horizon. Blood tests like the GALAD score (which looks at gender, age, AFP, DCP, and AFP-L3) can detect early cancer with 85% accuracy. They’re not yet standard, but they’re coming.
Eventually, we may move away from fixed schedules. Instead, your screening frequency could be personalized: every 3 months if your risk is high, every 12 months if it’s low, or even stopped if your liver fully regenerates.
But until then, stick to the basics. Know your history. Get scanned. Stay alive.
What Happens If You Skip Screening?
Liver cancer doesn’t come with warning signs-at least not in the early stages. By the time you feel pain, lose weight, or notice yellowing skin, the cancer is often advanced.
Early-stage liver cancer can often be treated with surgery, ablation, or targeted therapy. Five-year survival rates can be over 70% if caught early.
But if it’s found late? Survival drops below 15%. That’s not a gamble you want to take.
And here’s the kicker: liver cancer treatment is expensive. Screening is cheap. One ultrasound costs less than $100 in most places. A liver transplant? Over $500,000.
Prevention isn’t just smarter-it’s cheaper.
Do I still need liver cancer screening after being cured of hepatitis C?
Yes-if you had advanced fibrosis (F3) or cirrhosis (F4) before treatment. Even though the virus is gone, the scar tissue remains and can still turn cancerous. Screening every six months with ultrasound is recommended for these patients. If you had little to no scarring, your risk is very low and routine screening isn’t needed.
Is liver cancer risk the same after DAA treatment versus interferon?
No significant difference. Studies show the reduction in liver cancer risk is similar whether you were treated with modern DAAs or older interferon-based therapies. The key factor isn’t the drug-it’s the level of liver scarring you had before treatment. Both types of treatment lower risk by about 70-80%.
Can fibrosis reverse after hepatitis C is cured?
Yes, especially in patients with F3 fibrosis. Many people see their liver stiffness improve over time after achieving SVR. Some even regress to F0-F2. This is why follow-up FibroScan tests are important-they help determine if your risk is dropping and whether you can safely extend screening intervals.
Why do European and American guidelines differ on post-SVR screening?
Europe recommends screening for all patients with F3 or F4 fibrosis, fearing that fibrosis can be misclassified as less severe than it is. The U.S. recommends screening only for those with confirmed cirrhosis (F4), arguing that F3 patients have very low risk and screening may cause more harm than good through false positives. Both sides agree on cirrhosis patients-but the debate centers on advanced fibrosis.
How often should I get screened after SVR?
If you had cirrhosis before treatment: every 6 months. If you had advanced fibrosis (F3) and your liver has improved since SVR: discuss switching to once a year. If your FibroScan reading is now below 9.5 kPa, your risk may be low enough for yearly screening. Never stop without talking to your doctor.
What if I can’t afford or access ultrasound screening?
Talk to your doctor about alternatives. Some clinics offer subsidized screenings. Blood tests like FIB-4 or the GALAD score can help monitor risk between scans. If ultrasound isn’t available, at least get regular blood work and clinical exams. Don’t skip follow-up entirely-your liver still needs attention.
Can I stop screening after 5 or 10 years if I’ve been cancer-free?
Not yet. Current guidelines say screening should continue indefinitely for those with cirrhosis. Even after 10 years of SVR, the risk doesn’t drop to zero. Research is ongoing, and future guidelines may change based on long-term data-but for now, don’t assume you’re safe just because you’ve gone years without cancer.



Comments (9)