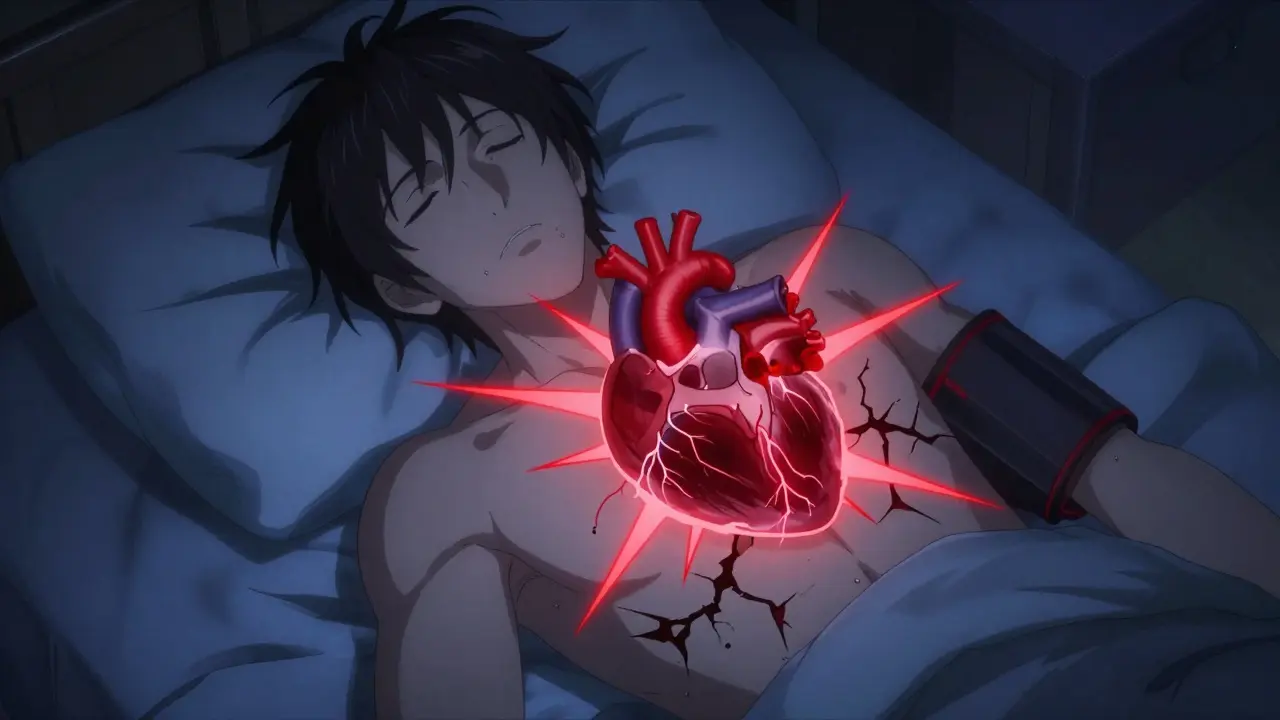
When you stop breathing for 10, 20, even 30 seconds while asleep, your heart doesn’t just pause-it panics. Every time this happens in obstructive sleep apnea (OSA), your body screams for oxygen. Your blood pressure spikes. Your heart races. Your electrical system stumbles. And if this happens dozens of times a night, every night, your heart starts to pay the price-sometimes in ways you won’t notice until it’s too late.
How Sleep Apnea Turns Nighttime Breathing Stops Into Heart Damage
Obstructive sleep apnea isn’t just loud snoring or feeling tired during the day. It’s a medical condition where your airway collapses repeatedly while you sleep, cutting off oxygen. Each time this happens, your brain jolts you awake-just enough to restart breathing, but not enough for real rest. These episodes can happen 5 times an hour (mild), 30 times (severe), or even more. And with every collapse, your body goes into survival mode. The moment oxygen drops, your sympathetic nervous system fires up like a siren. This is the same system that makes your heart pound when you’re scared. In OSA, it’s triggered every 1 to 3 minutes all night long. The result? Blood pressure spikes by 20 to 40 mmHg during each apnea. That’s like slamming your brakes hard over and over. Over time, your arteries don’t get a chance to relax. Your blood pressure stays high-even during the day. Studies show that 30 to 40% of people with high blood pressure have undiagnosed sleep apnea. And here’s the kicker: treating OSA can lower systolic pressure by 5 to 10 mmHg on average. That’s as effective as some blood pressure meds.The Link Between Sleep Apnea and Irregular Heartbeats
Your heart doesn’t just struggle with pressure-it starts misfiring. Sleep apnea is one of the strongest known triggers for atrial fibrillation (AFib), the most common type of dangerous arrhythmia. People with severe OSA are 3 to 5 times more likely to develop AFib than those without it. Why? Because the repeated oxygen drops and pressure swings create chaos in your heart’s electrical system. During an apnea, your heart gets squeezed by sudden changes in chest pressure. Then, when you gasp for air, blood surges back into your heart like a flood. This stretches the upper chambers, especially the left atrium. Over months and years, this leads to scarring and fibrosis. A 2024 study using cardiac MRI found OSA patients had more than twice the amount of atrial scarring compared to people without sleep apnea. That scar tissue is what causes erratic electrical signals-leading to AFib. The numbers are startling. While high blood pressure increases AFib risk by about 50%, severe sleep apnea bumps it up by 140%. And it’s not just AFib. Ventricular arrhythmias, heart block, and even sudden cardiac death are more common in untreated OSA. The American Heart Association now lists OSA as a Class I risk factor for AFib-same level as obesity and hypertension. That means doctors should treat it like a direct cause, not just a side note.Why Sleep Apnea Is Worse Than You Think
Many people assume that if they’re young, fit, or not overweight, they’re safe from OSA. That’s a dangerous myth. New research from UT Southwestern Medical Center (2024) shows that even adults under 40 with untreated sleep apnea face significantly higher heart risks. You don’t have to be obese or elderly. Men with narrow airways, women after menopause, people with a thick neck, or even those with a family history are at risk. And here’s what most don’t realize: OSA doesn’t just make heart problems worse-it causes them independently. Even after controlling for obesity, diabetes, smoking, and age, studies still show OSA increases stroke risk by 60%, coronary artery disease by 30%, and heart failure by 140%. It’s not just a side effect. It’s a root cause. Think of it this way: if you had a leaky pipe in your basement that dripped every few minutes, you wouldn’t wait until the walls collapsed to fix it. Sleep apnea is that leak. The damage builds slowly, silently. By the time you feel tired or notice your heart skipping beats, your heart may already be structurally changed.
What Happens When You Treat It
The good news? The damage isn’t always permanent. Continuous Positive Airway Pressure (CPAP) therapy-the most common treatment-works. It’s not magic, but it’s science-backed. CPAP keeps your airway open with gentle air pressure, stopping apneas before they start. A 2024 study of over 5,200 CPAP users found that 65% reduced their blood pressure medication needs after consistent use. Those who used CPAP 4+ hours a night saw their AFib episodes drop from weekly to once every 2-3 months. One user, diagnosed with severe OSA (AHI of 42), reported his blood pressure falling from 160/95 to 128/82 within three months. CPAP doesn’t just help your heart-it helps your whole body. It lowers inflammation, reduces oxidative stress, improves endothelial function, and resets your autonomic nervous system. After 12 months of consistent use, AFib recurrence drops by 42%. That’s not a small benefit. That’s a game-changer.Why So Many People Don’t Stick With Treatment
But here’s the catch: most people quit. About 25 to 30% stop using CPAP within the first year. Common complaints? Mask discomfort, dry mouth, claustrophobia, and noise. But these aren’t reasons to give up-they’re problems to solve. Modern CPAP machines have features to help: ramp mode (slow pressure increase), heated humidifiers, nasal pillows instead of full-face masks, and quieter motors. Many users adapt within 2-4 weeks. And 85% say their sleep quality improves noticeably after 30 days of consistent use. If you’re struggling, talk to your sleep specialist. There are alternatives: oral appliances for mild cases, weight loss (even 10% can cut apneas in half), positional therapy (sleeping on your side), or newer options like hypoglossal nerve stimulation (Inspire Therapy), which acts like a pacemaker for your airway. It’s implanted, but studies show a 79% drop in apnea events.
Who Should Get Screened-and How
If you have high blood pressure, atrial fibrillation, heart failure, or a stroke, you should be tested for sleep apnea. The American Academy of Sleep Medicine says 45 to 65% of these patients have undiagnosed OSA. Yet only 20 to 25% of at-risk people are even screened. Testing is easier than ever. Home sleep tests are now accurate for most cases. You wear a small device overnight that tracks breathing, oxygen levels, and heart rhythm. It’s not as detailed as an overnight lab study, but for 80% of people, it’s enough to confirm OSA. Diagnosis requires an Apnea-Hypopnea Index (AHI) of 5 or more events per hour. Mild: 5-14. Moderate: 15-29. Severe: 30+. If you snore loudly, gasp for air at night, wake up with headaches, or feel exhausted despite 8 hours in bed, your AHI is probably higher than you think.What You Can Do Today
You don’t need to wait for a doctor’s appointment to start protecting your heart. If you suspect sleep apnea:- Ask your partner if you stop breathing while sleeping.
- Track your blood pressure at home. If it’s high and doesn’t respond to meds, OSA could be the cause.
- Use a sleep tracking app or wearable (like Apple Watch or Fitbit) to monitor oxygen drops and heart rate spikes at night.
- Try sleeping on your side. Many people breathe better this way.
- Reduce alcohol before bed-it relaxes throat muscles and worsens apneas.
- Get tested. Seriously. If you have heart disease, you’re overdue for this check.
Final Thought: Your Heart Doesn’t Sleep
Your heart works 24/7. When sleep apnea steals your rest, it doesn’t just make you tired-it makes your heart work harder, faster, and under stress. Every night you go untreated, you’re slowly wearing down your cardiovascular system. But the reverse is true too. Fix your breathing at night, and your heart gets a second chance. Blood pressure drops. Arrhythmias fade. Medications become easier to manage. Energy returns. The science is clear. The tools exist. The choice is yours.Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity is a common risk factor, sleep apnea can occur in people of any weight. Narrow airways, jaw structure, hormonal changes (especially after menopause), and genetics can all cause OSA. The mechanical stress from repeated breathing stops directly raises blood pressure by triggering the nervous system-regardless of body weight. Studies show 30-40% of people with high blood pressure have undiagnosed sleep apnea, even if they’re not overweight.
Does treating sleep apnea reduce the risk of heart attack?
Yes. Consistent use of CPAP therapy reduces the risk of heart attack and other cardiovascular events by lowering blood pressure, reducing inflammation, and stabilizing heart rhythm. One study found that people with severe OSA who used CPAP regularly had a 40-50% lower risk of major heart events compared to those who didn’t treat it. The American Heart Association now treats OSA as a direct contributor to heart disease, not just a side condition.
Is CPAP the only treatment for sleep apnea?
No. CPAP is the most common and effective treatment, especially for moderate to severe cases. But alternatives include oral appliances (for mild to moderate OSA), weight loss (even 10% can improve symptoms), positional therapy (sleeping on your side), and surgery to remove excess tissue. For those who can’t tolerate CPAP, hypoglossal nerve stimulation (Inspire Therapy) is an implanted device that stimulates the airway muscle during sleep. It’s been shown to reduce apnea events by 79% in clinical trials.
How long does it take for CPAP to improve heart health?
Some improvements happen quickly. Blood pressure can drop within weeks of consistent use. Atrial fibrillation episodes often decrease noticeably after 3-6 months. For long-term heart protection-like reducing scarring and inflammation-it takes 12 months or more of regular use (4+ hours per night). The key is consistency, not perfection. Even 4 hours a night, 5 nights a week, makes a measurable difference.
Can sleep apnea cause sudden cardiac death?
Yes. Untreated severe sleep apnea increases the risk of sudden cardiac death, especially during nighttime hours when breathing stops are most frequent. The combination of low oxygen, high blood pressure spikes, and electrical instability in the heart creates the perfect storm for dangerous arrhythmias. Studies show people with severe OSA are 2-3 times more likely to die suddenly from heart-related causes than those without it. Treating OSA significantly reduces this risk.
Should I get tested for sleep apnea if I have atrial fibrillation?
Absolutely. Between 45% and 60% of people with atrial fibrillation also have undiagnosed sleep apnea. In fact, OSA is one of the strongest predictors of AFib recurrence after procedures like ablation. Treating sleep apnea can reduce AFib episodes by up to 42% and improve the success of heart rhythm treatments. If you have AFib, getting tested for OSA isn’t optional-it’s part of your heart care plan.


Comments (9)