Opioid Monitoring Risk Calculator
Assess Your Opioid Monitoring Risk
This tool helps determine appropriate urine drug testing frequency based on the Opioid Risk Tool (ORT) criteria. It's designed to help clinicians and patients make informed decisions about monitoring safety.
Risk Assessment Results
Recommended Testing Frequency
Key Recommendations
When patients are prescribed opioids for chronic pain, doctors aren’t just trying to manage pain-they’re trying to keep them alive. Opioids save lives when used correctly, but they also carry a serious risk of misuse, overdose, and death. That’s why urine drug screens and risk stratification have become essential tools in modern opioid treatment. These aren’t just bureaucratic checks. They’re clinical lifelines.
Why Urine Drug Screens Are Standard Practice
Urine drug testing isn’t new. It started in addiction treatment centers decades ago, but by the 2010s, it became a routine part of opioid therapy for chronic pain. The CDC, ASAM, and AAFP all now recommend it. Why? Because self-reports are unreliable. Patients might forget, misunderstand, or hide use. A urine test gives objective data. The goal isn’t to catch people doing something wrong. It’s to catch things that could kill them. In 2021, over 80,000 drug overdose deaths in the U.S. involved opioids. Many of those deaths happened because patients were mixing prescribed opioids with other substances-like benzodiazepines, alcohol, or illicit fentanyl-without their doctor knowing. Urine tests help spot those hidden risks. They confirm whether the patient is taking their prescribed medication. They also reveal if they’re using something they didn’t tell the doctor about. That’s critical. Fentanyl, for example, is 50 to 100 times stronger than morphine. A patient on a low-dose oxycodone prescription might not realize they’re at risk-until they test positive for fentanyl.How Urine Tests Work: Screening vs. Confirmation
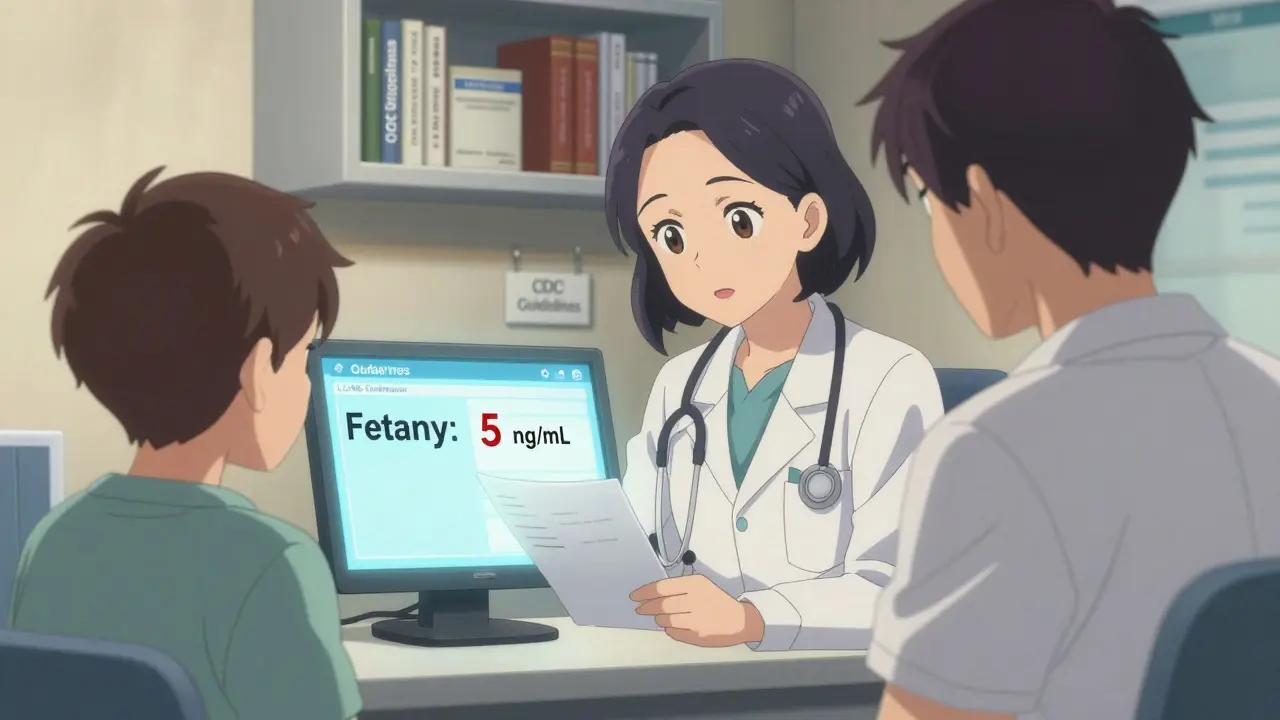
Not all urine tests are the same. There are two main types: screening and confirmation. Screening tests, like immunoassays (EMIT, TDx), are fast and cheap-around $5 per test. They give results in hours. But they’re not perfect. Up to 30% of results can be false positives. Common over-the-counter meds like ibuprofen, poppy seeds, or even some cough syrups can trigger a positive for opioids. And here’s the bigger problem: many standard screens don’t detect fentanyl at all. That’s because fentanyl doesn’t look like morphine under the test’s chemical sensors. That’s where confirmation testing comes in. Gas Chromatography/Mass Spectrometry (GC/MS) or Liquid Chromatography/Mass Spectrometry (LC-MS) are the gold standards. They cost $25 to $100 per test, take days, and are billed differently to Medicare. But they’re accurate. They don’t just say “opiate positive.” They say “oxycodone at 1,200 ng/mL” or “fentanyl at 5 ng/mL.” One of the biggest clinical surprises? Hydrocodone. Studies show that in 72% of cases where patients were taking hydrocodone, their initial urine screen came back negative. Why? Because many immunoassays are designed to detect morphine, not hydrocodone. If a doctor sees a negative result and assumes non-adherence, they might reduce the dose-or worse, cut it off entirely. That’s dangerous.The Fentanyl Blind Spot
Fentanyl is the silent killer in opioid monitoring. Even in 2025, many clinics still use outdated panels that miss it. That’s why the FDA approved the first fentanyl-specific immunoassay in 2023. It detects fentanyl at levels as low as 1 ng/mL with 98.7% accuracy. But adoption is slow. Many labs haven’t switched yet. Clinicians report real-world problems. One doctor in Ohio said, “I had a patient on a fentanyl patch who tested negative three times. I thought she was diverting. Turned out the lab just didn’t test for fentanyl. She was terrified I’d accuse her of lying.” This isn’t just about accuracy-it’s about trust. When patients feel like they’re being policed instead of cared for, they disengage. That’s why labs and clinics are moving toward more targeted testing: if a patient is on fentanyl, the test must include fentanyl.Who Needs Testing and How Often?
You don’t test everyone the same way. That’s where risk stratification comes in. The Opioid Risk Tool (ORT) is a simple 5-question screening used in clinics. It asks about family history of substance use, personal history of preadolescent sexual abuse, history of alcohol or drug abuse, and psychiatric disorders. Based on the score, patients are grouped into low, moderate, or high risk. - Low risk: Annual urine test. No red flags. Stable pain, no history of misuse. - Moderate risk: Every 6 months. Maybe a history of anxiety or occasional alcohol use. - High risk: Every 3 months. Past opioid use disorder, multiple prescriptions, or recent overdose. This isn’t punishment. It’s precision. High-risk patients need more frequent checks because their chance of overdose is 5 to 10 times higher. But low-risk patients don’t need monthly tests. That’s wasteful and erodes trust. A 2023 study in JAMA showed clinics using this tiered approach reduced unnecessary testing by 40% and improved patient satisfaction by 32%.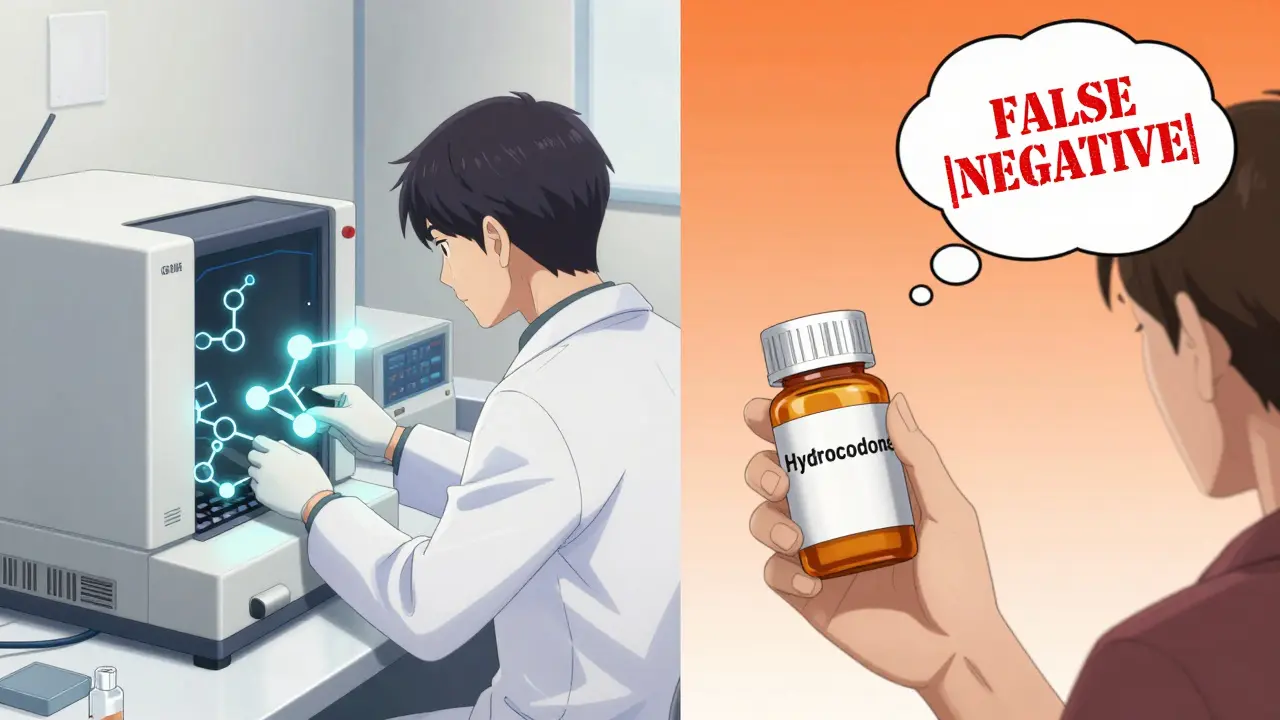
What the Test Can’t Tell You
A lot of myths surround urine drug screens. Here’s what they don’t do:- They don’t measure pain levels.
- They don’t tell you if the dose is “right.”
- They don’t prove someone is addicted.
- They can’t detect alcohol, nicotine, or caffeine reliably.
Specimen Validity: Spotting Tampering
Some patients try to beat the test. They dilute urine with water. They add bleach or vinegar. They bring someone else’s urine. Most labs now check for validity:- Specific gravity: Below 1.003? Likely diluted.
- pH: Below 4.5 or above 9.0? Possible adulteration.
- Creatinine: Below 20 mg/dL? Probably substituted.
What’s Changing in 2025
The field is evolving fast. - The CDC’s updated guidelines (expected late 2024) will require LC-MS for patients on synthetic opioids like fentanyl, carfentanil, or nitazenes. - Point-of-care devices are in FDA review. In the next 2 years, some clinics may get lab-quality results in under 20 minutes. - AI tools are being tested to predict adherence. One model from the University of Pittsburgh, called OAPE, analyzes test history, prescription patterns, and behavioral data to flag high-risk patients before they overdose. - Insurance and Medicare are shifting reimbursement. Basic immunoassays are still covered, but labs are being pushed to use targeted panels instead of blanket screens.
Real Impact: Stories From the Clinic
A nurse practitioner in Arizona started using risk-stratified testing in 2022. She had a patient-a 58-year-old with spinal stenosis-on oxycodone. He tested negative for oxycodone twice. She was ready to cut him off. Then she ordered a confirmatory test. It showed oxycodone. Why the false negative? The lab used an outdated immunoassay that didn’t detect oxycodone metabolites. She didn’t punish him. She switched labs. He stayed on therapy. His pain improved. He stopped using alcohol. Another clinic in Pennsylvania reduced lost prescriptions by 37% after implementing quarterly testing for high-risk patients. They didn’t fire anyone. They just started asking, “What’s going on?” instead of “You’re lying.”What Clinicians Get Wrong
The biggest mistake? Treating a negative test as proof of non-compliance. A 2022 survey of 1,247 pain doctors found 68% had seen false-negative hydrocodone results at least once a month. Nearly half of those doctors had considered reducing or stopping therapy because of it. That’s dangerous. Another mistake? Testing too often. A patient with no history of misuse, stable pain, and no other substance use doesn’t need a test every 3 months. That’s not monitoring. That’s surveillance. And finally: don’t use urine tests to judge someone’s character. They’re not moral tests. They’re medical tools.What Patients Should Know
If you’re on long-term opioids:- Urine tests aren’t about distrust. They’re about safety.
- Ask what drugs the test checks for-especially if you’re on fentanyl or hydrocodone.
- If you test negative but know you took your medicine, ask for a confirmatory test.
- Don’t hide other medications. Even OTC ones can interfere.
- Your test results are private. They’re not shared with employers or law enforcement unless you’re in a court-mandated program.
Final Thoughts
Urine drug screens and risk stratification aren’t perfect. But they’re the best tools we have right now to prevent overdose deaths in patients on long-term opioid therapy. The goal isn’t to control patients. It’s to protect them. The future of opioid monitoring isn’t more testing. It’s smarter testing. Targeted. Accurate. Respectful. And above all-human.Are urine drug tests required by law for opioid patients?
Thirty-eight U.S. states require urine drug screening for patients on chronic opioid therapy, especially if doses exceed certain thresholds. But requirements vary by state and provider type. In most cases, testing is mandated by clinical guidelines-not criminal law. It’s a medical standard, not a legal punishment.
Can I be fired or denied care for a positive drug test?
In most cases, no. If you’re taking prescribed opioids and the test shows only those medications, you’re not at risk. If illicit substances are found, your provider will discuss options-not immediately cut you off. The goal is harm reduction. Discontinuing opioids abruptly can cause withdrawal, increased pain, or even suicide. Most clinics work with patients to adjust treatment, not punish them.
Why do some opioid tests miss hydrocodone or fentanyl?
Standard immunoassay tests are designed to detect morphine-like structures. Hydrocodone and fentanyl have different chemical shapes, so they often don’t trigger the test. Many labs still use outdated panels. That’s why confirmatory testing with GC/MS or LC-MS is critical for patients on these drugs. Always ask your lab what’s included in the panel.
Is it better to use blood instead of urine for opioid testing?
No. Urine is preferred because it’s noninvasive, cheaper, and detects drug use over a longer window (1-3 days). Blood tests only show recent use (hours), which doesn’t help assess adherence. Blood is only used in emergencies-like suspected overdose or trauma.
Do urine tests detect marijuana if I’m on opioids?
Yes, if the panel includes cannabinoids. Most standard opioid monitoring panels now test for THC, because mixing marijuana with opioids increases sedation and overdose risk. Synthetic cannabinoids (like Spice or K2) are harder to detect and often require special testing.
How accurate are new fentanyl-specific urine tests?
The new FDA-approved fentanyl immunoassay (Immunalysis Fentanyl EIA) has 98.7% sensitivity at detecting fentanyl at 1 ng/mL. That’s nearly perfect. But it’s still new. Not all labs have switched. If you’re on a fentanyl patch and your test keeps coming back negative, ask for a confirmatory LC-MS test.
Can I refuse a urine drug test?
Yes, but refusing may lead your provider to stop prescribing opioids. That’s because they can’t safely monitor your treatment without objective data. It’s not about control-it’s about risk. If they can’t confirm you’re not mixing opioids with other dangerous substances, continuing therapy could be unsafe.



Comments (10)