Every year, tens of thousands of people in the U.S. die from opioid overdoses. Most of these deaths aren’t inevitable. They happen because no one nearby knows how to respond - or worse, they’re afraid to act. The truth is simple: if you have someone at risk of an opioid overdose, you need naloxone. Not just as a backup, but as something you keep within reach, like a fire extinguisher. And you need to know how to use it, when to use it, and how to store it so it actually works when it matters.
What Naloxone Does - And What It Doesn’t
Naloxone is not a cure. It’s not a painkiller. It doesn’t make you feel better. It’s a switch. When someone overdoses on opioids - whether it’s heroin, oxycodone, fentanyl, or even prescription pills - their breathing slows or stops. Their brain can’t get oxygen. Naloxone slams into the same receptors in the brain that the opioids are stuck to, yanks them out, and flips the breathing switch back on. In under five minutes, if given right, the person starts breathing again.
It’s not magic. It doesn’t work on alcohol, benzodiazepines, cocaine, or meth. If someone overdoses on a mix of drugs and opioids, naloxone will only help with the opioid part. But since fentanyl is so common now - involved in over 80% of opioid overdose deaths in 2022 - naloxone is often the only thing standing between life and death.
And it’s incredibly safe. If you give naloxone to someone who hasn’t taken opioids, nothing happens. No side effects. No danger. That’s why it’s legal to carry without a prescription in every state. You can’t accidentally harm someone by giving it. The only real risk is if you give too much to someone who’s been using opioids regularly. They might go into sudden withdrawal - shaking, vomiting, sweating, angry. It’s terrifying to watch, but it’s not deadly. And it’s far better than watching someone stop breathing.
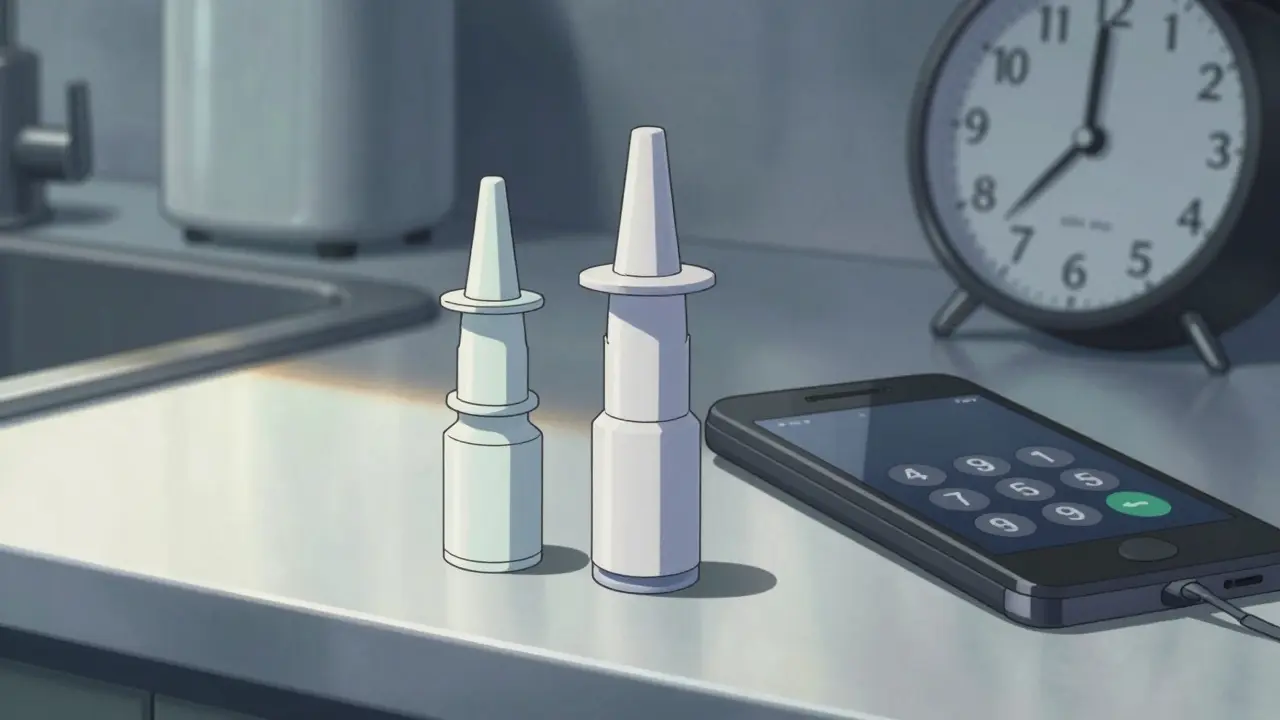
How Naloxone Is Given - Nasal Spray vs. Injection
There are two main ways to give naloxone: nasal spray and injection. The nasal spray - sold as Narcan - is the most common today. It’s easy. No needles. No training needed beyond the printed instructions. You tilt the person’s head back, insert the nozzle into one nostril, and press the plunger. That’s it. The spray delivers the drug into the nasal lining, where it gets absorbed into the bloodstream.
Studies show nasal spray works just as well as injection when used correctly. In fact, community users had an 85% success rate with nasal spray versus 78% with injection, mostly because people froze up with the needle. The newer version of Narcan, approved in 2023, delivers 4 mg of naloxone - double the old dose - which is critical because fentanyl is so strong. Many overdoses now need two doses, sometimes three.
Injectable naloxone is still used by EMS and hospitals. It’s cheaper, but harder to use in a panic. You need a syringe, alcohol wipe, and the right technique. For most people - family members, friends, neighbors - nasal spray is the clear choice.
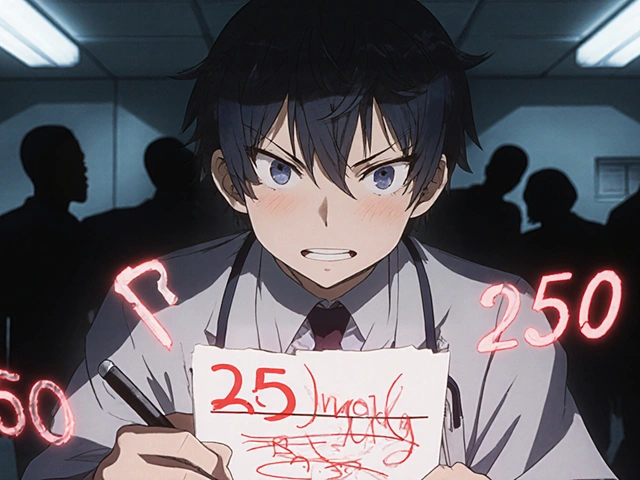
Why One Dose Often Isn’t Enough
Here’s where people get caught off guard. Naloxone lasts 30 to 90 minutes. Fentanyl? It can last 4 to 8 hours. That means after naloxone wears off, the opioid is still in the body. The person can slip back into overdose. This is called re-narcotization. In 2022, the CDC found that 40% of fentanyl overdose reversals needed more than one dose of naloxone.
That’s why calling 911 isn’t optional. Even if they wake up, you need medical help. They need to be monitored for at least two hours. Some people have been discharged after one dose, only to collapse again an hour later. Don’t assume they’re safe just because they’re breathing. Stay with them. Keep the second dose ready.
How to Store Naloxone So It Actually Works
Storing naloxone wrong is like keeping a fire extinguisher in the garage during winter. It might look fine - but when you need it, it’s useless.
Naloxone should be kept at room temperature - between 68°F and 77°F (20°C to 25°C). It can handle short trips in the car, but don’t leave it in a hot glovebox or freezing trunk. Sunlight breaks it down. Heat makes it weaker. If the liquid inside the nasal spray looks cloudy or has particles, don’t use it. Throw it out and get a new one.
Keep it where you can find it fast. Not in a locked cabinet. Not buried in a drawer. Keep it with your keys, in your purse, or taped to the inside of your medicine cabinet. If you live with someone who uses opioids, put it in a spot you both know - even better, put one in their car and one in your home. Make sure everyone who might be around them knows where it is.
Check the expiration date every six months. Most kits expire in two years. If it’s close, replace it. Many community programs give out free naloxone. Call your local health department or visit NIDA’s website - they can send you a kit at no cost.
Recognizing an Overdose - It’s Not Always Obvious
People think overdoses look like someone passed out on the floor. Sometimes they do. But often, it’s subtler. Look for these signs:
- Slow, shallow, or stopped breathing
- Blue or gray lips and fingernails
- Unresponsiveness - shaking them, shouting, rubbing their sternum - no reaction
- Pinpoint pupils (tiny dots in the center of the eyes)
- Gurgling or snoring sounds - like they’re drowning in their own saliva
If you’re unsure, give naloxone anyway. The worst case? You give it to someone who didn’t need it. The best case? You save a life.

What to Do After Giving Naloxone
After you give the spray:
- Call 911 immediately. Don’t wait. Say, “Someone overdosed on opioids. I gave naloxone.”
- Put the person on their side in the recovery position. This keeps their airway open if they vomit.
- Stay with them. Watch their breathing. If they don’t respond in 2-3 minutes, give a second dose in the other nostril.
- Even if they wake up, don’t let them leave. They need to be evaluated by medical staff.
Don’t be afraid of the withdrawal. People scream, kick, cry. They might try to run. Hold them gently. Talk to them. Say, “You’re safe. Help is coming.”
Cost, Access, and Myths
Naloxone nasal spray costs $130-$150 at pharmacies without insurance. That’s expensive. But here’s the thing: you don’t have to pay. Most states have free distribution programs through pharmacies, clinics, or community groups. In Melbourne, Australia, similar programs exist through local health services and needle exchanges. Ask your pharmacist - they can point you to free kits.
Myth: “Giving naloxone encourages drug use.” No. Studies show communities that hand out naloxone don’t see more drug use. They see fewer deaths. The American Heart Association, CDC, and WHO all agree: saving lives comes first.
Myth: “I’ll get in trouble for giving it.” You won’t. All 50 U.S. states have Good Samaritan laws that protect people who call for help during an overdose. Same goes for Australia. You’re doing the right thing.
What’s Next for Naloxone
Scientists are working on longer-lasting versions. One new drug, nalmefene, lasts up to 11 hours and might replace naloxone in the future. But right now, naloxone is still the only thing widely available. And it’s enough.
The Biden administration is spending $200 million to get 2 million naloxone kits into homes, schools, and public spaces by 2026. That’s progress. But the real change happens when one person - you - decides to carry it.
You don’t need to be a doctor. You don’t need to be brave. You just need to be ready.
Can naloxone be used for children or pregnant women?
Yes. Naloxone is safe for children, pregnant women, and elderly people. It doesn’t cross the placenta in harmful amounts, and it doesn’t cause long-term side effects. If a child overdoses on opioids - even accidentally swallowing a pill - give naloxone and call 911. The risk of not acting is far greater than any potential side effect.
How long does naloxone take to work?
Naloxone usually starts working in 2 to 5 minutes when given as a nasal spray. If there’s no response after 3 minutes, give a second dose. Some people respond faster - especially if they’ve taken a smaller dose of opioids. But with fentanyl or carfentanil, it can take longer. Don’t wait more than 5 minutes to give a second dose if they’re still not breathing.
Is naloxone effective against fentanyl?
Yes, but you often need more of it. Fentanyl is 50 to 100 times stronger than morphine. One standard dose of naloxone (2 mg) may not be enough. The newer 4 mg nasal spray was designed for this. Many reversals now require two or three doses. Always assume fentanyl is involved if you’re unsure - and be ready to give more than one dose.
Can I reuse a naloxone nasal spray?
No. Each nasal spray is single-use. Once you press the plunger, the device is done. Even if you only give half the dose, you can’t save it for later. Always carry at least two kits if you’re around someone at risk. Some kits come with two sprays - that’s ideal.
Where can I get free naloxone?
In the U.S., most pharmacies offer free naloxone with a standing order - no prescription needed. You can also get it from local health departments, harm reduction centers, syringe exchanges, and nonprofits like the Harm Reduction Coalition. In Australia, naloxone is available free through community health services and needle and syringe programs. Search “free naloxone near me” or call your local public health office.
What if I’m scared to use naloxone?
It’s normal to be scared. But you don’t need to be perfect. Even if you’re shaky, even if you’re crying, just follow the instructions on the box. Tilt the head, insert the nozzle, press. That’s all. Thousands of people have saved lives this way - with no training, just courage. You’re not responsible for fixing their addiction. You’re responsible for keeping them alive long enough to get help.



Comments (10)