If you drink pomegranate juice for its antioxidants and tart sweetness, you might be wondering: is it safe with your meds? The answer isn’t simple. Some studies say it’s fine. Others warn of serious risks. And doctors don’t all agree. But here’s what matters: pomegranate juice can change how your body processes certain medications - and that could be dangerous.
How Pomegranate Juice Interacts With Your Meds
Pomegranate juice doesn’t just add flavor to your breakfast. It contains compounds like punicalagins and ellagitannins that can block enzymes in your liver and gut. These enzymes - especially CYP3A4 and CYP2C9 - are responsible for breaking down about 60% of the prescription drugs people take daily. When they’re slowed down, your body doesn’t clear the medicine as fast. That means more of it builds up in your bloodstream. This isn’t just theory. In lab tests, pomegranate juice has been shown to inhibit CYP3A4 by 20-50% and CYP2C9 by up to 40%. That’s similar to what grapefruit juice does - but grapefruit has clear FDA warnings. Pomegranate doesn’t. Why? Because human studies don’t always back up the lab results.The Warfarin Warning: A Real Risk
The clearest danger is with warfarin, a blood thinner used to prevent strokes and clots. Warfarin has a very narrow safety window. Too little, and you risk a clot. Too much, and you could bleed internally. Even small changes in blood levels can be life-threatening. Case reports show real problems. One patient’s INR - a measure of blood clotting time - jumped from 2.4 to 4.7 after drinking a daily glass of pomegranate juice. That’s a 96% increase in blood-thinning effect. The doctor had to reduce their warfarin dose by 30% to get it back under control. The European Medicines Agency and Mayo Clinic both say: if you’re on warfarin, monitor your INR more closely when you start or stop drinking pomegranate juice. Some experts recommend avoiding more than 8 ounces a day. Others say consistency matters more than avoidance - meaning if you’ve been drinking it for months, don’t suddenly quit. The shock of stopping could be just as risky as starting.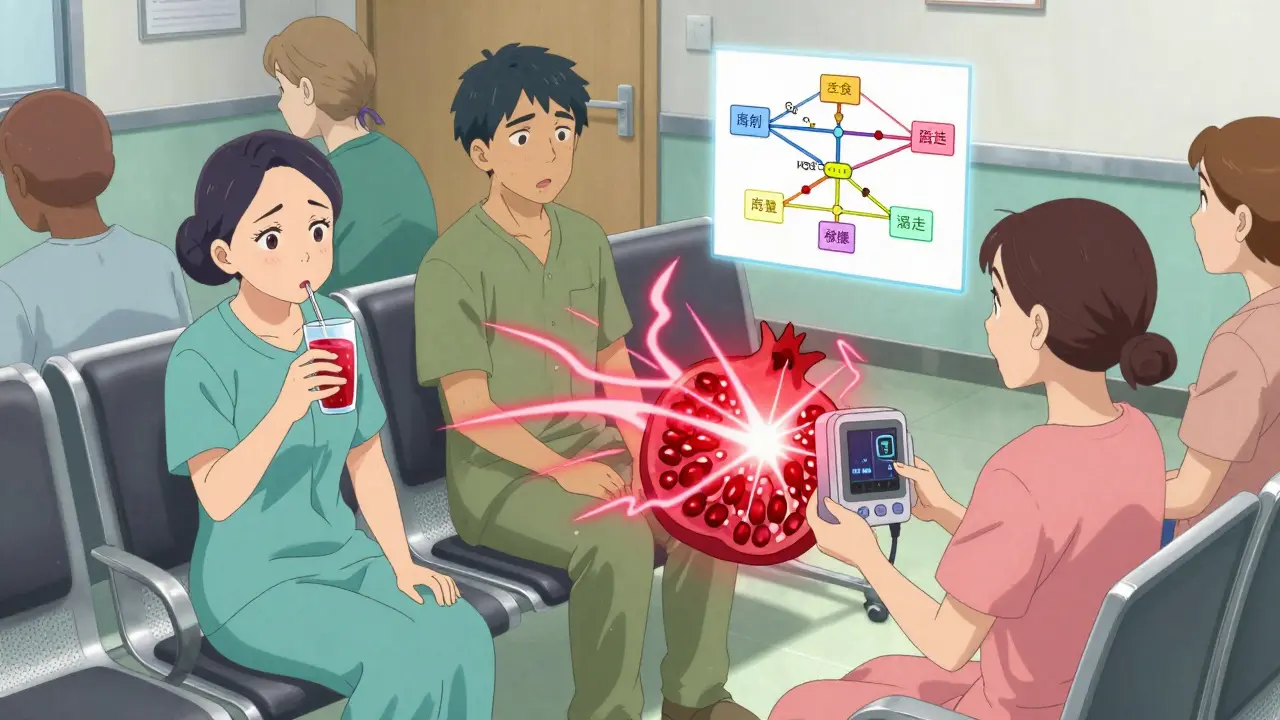
Not All Medications Are Affected
Here’s the good news: most people taking pomegranate juice won’t have issues. A 2022 survey of over 1,200 patients found that only 4.7% experienced any possible interaction. Most of those were on warfarin. Studies on other drugs show mixed results. One trial gave 12 healthy volunteers 330 mL of pomegranate juice daily for two weeks while they took midazolam, a drug processed by CYP3A4. No change in blood levels. Another study on theophylline (used for asthma) found only a 7.2% increase in drug exposure - far below the 25-40% threshold that doctors consider clinically meaningful. Drugs like atorvastatin (Lipitor), quetiapine (Seroquel), and some ACE inhibitors (like lisinopril) are listed as having “moderate” interactions with pomegranate juice on WebMD. But real-world data is thin. No major hospital system has banned pomegranate juice for patients on these drugs - unlike grapefruit, which is often strictly avoided with statins.Why the Confusion?
The big problem? Lab tests and real life don’t match. In a test tube, pomegranate juice blocks enzymes hard. In your body? It’s messy. Your gut absorbs it differently. Your liver processes it differently. And your genes matter. Some people have natural variations in CYP2C9 or CYP3A4 that make them more or less sensitive to these effects. A 2023 review of 27 studies concluded: “While lab data strongly suggest inhibition, human evidence remains inconsistent.” Only warfarin has enough case reports to suggest a real, measurable risk. For everything else? It’s a maybe. The FDA doesn’t require warning labels on pomegranate juice. They do for grapefruit. Why? Because grapefruit has been proven to spike statin levels by up to 15 times in some people. Pomegranate juice? The highest increase seen in human trials was under 40% - and even that wasn’t consistent.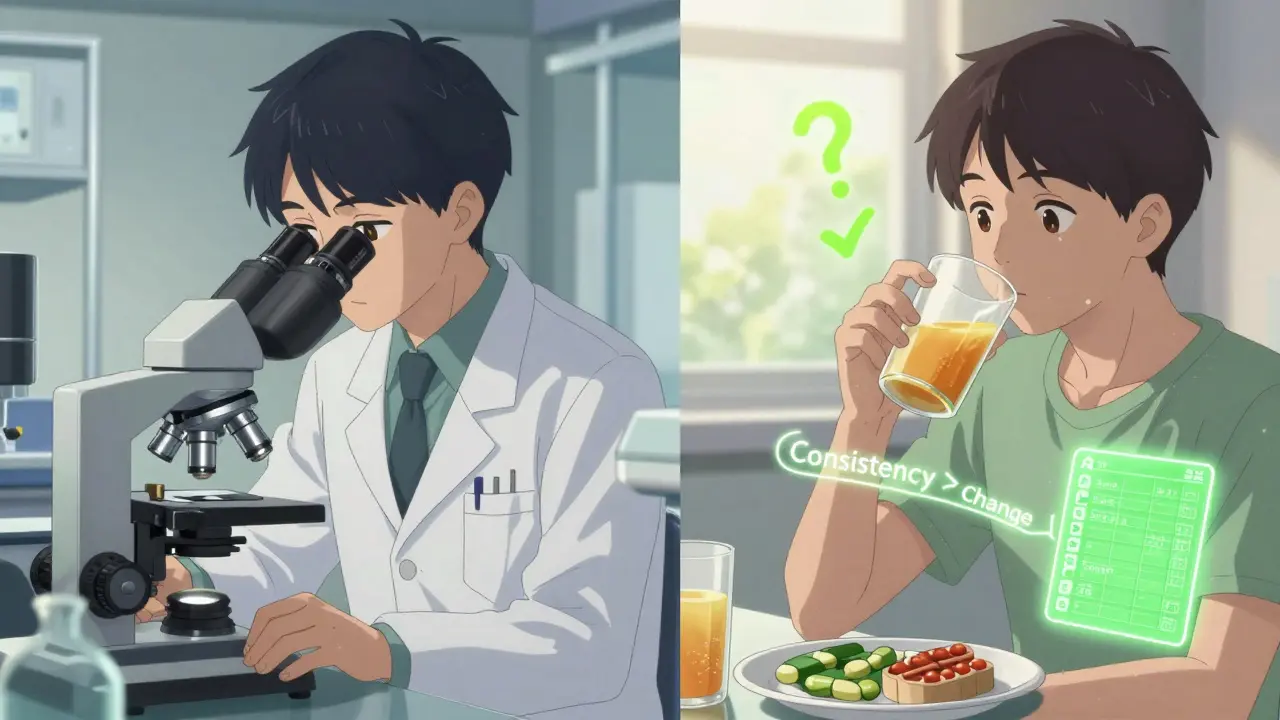
What Should You Do?
If you take any medication regularly, here’s your practical plan:- Check your meds. Look up your specific drugs on Mayo Clinic’s Drug Interaction Checker or ask your pharmacist. Warfarin, some antidepressants, and certain heart meds are the main ones to watch.
- Be consistent. If you drink pomegranate juice, keep doing it the same amount every day. Don’t start, stop, or change your intake without telling your doctor. Sudden changes are riskier than steady use.
- Time it right. If you’re concerned, wait at least two hours between taking your pill and drinking the juice. That reduces the chance of direct interaction in your gut.
- Monitor if you’re on warfarin. Get your INR checked more often when you begin or stop drinking pomegranate juice. Don’t wait for symptoms like bruising or nosebleeds.
- Don’t panic. For most people, a glass a day isn’t a problem. The real danger comes from mixing it with high-risk drugs and ignoring changes in how you feel.
What’s Next?
Researchers are still digging. The National Institutes of Health is funding a study tracking 150 people taking pomegranate juice with 12 common medications - results are due in late 2024. Another study is looking at whether your genes make you more vulnerable. That could lead to personalized advice someday. For now, the advice is simple: know your meds. Know your habits. Talk to your doctor or pharmacist before making big changes. You don’t have to give up pomegranate juice - but you do need to be smart about it.Can pomegranate juice interact with blood thinners like warfarin?
Yes. There are documented cases where regular pomegranate juice consumption raised INR levels in people taking warfarin, increasing the risk of bleeding. While not everyone experiences this, the effect is strong enough that doctors recommend increased INR monitoring when starting or stopping pomegranate juice. Consistency in intake is safer than sudden changes.
Is pomegranate juice as dangerous as grapefruit juice?
No. Grapefruit juice is known to dramatically increase blood levels of certain drugs - sometimes by 15 times - and the FDA has issued clear warnings. Pomegranate juice has a much weaker effect in humans. While it can inhibit drug-metabolizing enzymes in lab tests, real-world studies show inconsistent results. Only warfarin has strong enough evidence to warrant caution.
Should I stop drinking pomegranate juice if I take medication?
Not necessarily. For most medications, moderate daily intake (like 8 ounces) is considered safe. The bigger risk comes from suddenly starting or stopping it, especially if you’re on a drug with a narrow therapeutic window like warfarin. Talk to your doctor first. They can advise based on your specific meds and health history.
Which medications are most likely to interact with pomegranate juice?
The most documented risk is with warfarin. Other possible interactions include certain statins (like atorvastatin), some antidepressants (like sertraline), antipsychotics (like quetiapine), and ACE inhibitors (like lisinopril). However, human evidence is limited for all except warfarin. Always check with your pharmacist or use a trusted drug interaction checker.
How long should I wait between taking medication and drinking pomegranate juice?
Pharmacists at the University of North Carolina recommend waiting at least two hours between taking your medication and consuming pomegranate juice. This reduces the chance of direct interaction in the gut, where many enzymes are inhibited. It’s a simple step that can lower risk without requiring you to give up the juice entirely.
Are there any benefits to drinking pomegranate juice with medication?
There’s no evidence that pomegranate juice improves how medications work. Its benefits - like antioxidants and anti-inflammatory effects - are separate from drug metabolism. Any potential benefit would be in overall health, not enhanced drug performance. The focus should be on avoiding harm, not seeking synergy.



Comments (14)