When your prescription switches from brand to generic, do you even notice?
Most people don’t think twice when their pharmacy hands them a pill that looks different from what they’ve been taking. But what if the generic wasn’t made by some unknown company-it was made by the same manufacturer as the brand-name drug? That’s an authorized generic. And surprisingly, more patients than you’d think prefer it.
Authorized generics aren’t just cheaper versions of brand-name drugs. They’re exact copies-same active ingredients, same inactive fillers, same factory, same packaging (minus the brand logo). The FDA calls them "products with no applicant" because they’re made under the original drug’s approval, not a new generic application. This means they’re chemically identical to the brand, down to the last molecule.
So why does this matter? Because when patients switch from a brand-name drug to a generic, some go back. They feel different. Their stomach acts up. Their headache doesn’t go away. Or they just don’t trust it. That’s where authorized generics step in-and they’re changing the game.
Why authorized generics feel more like the brand
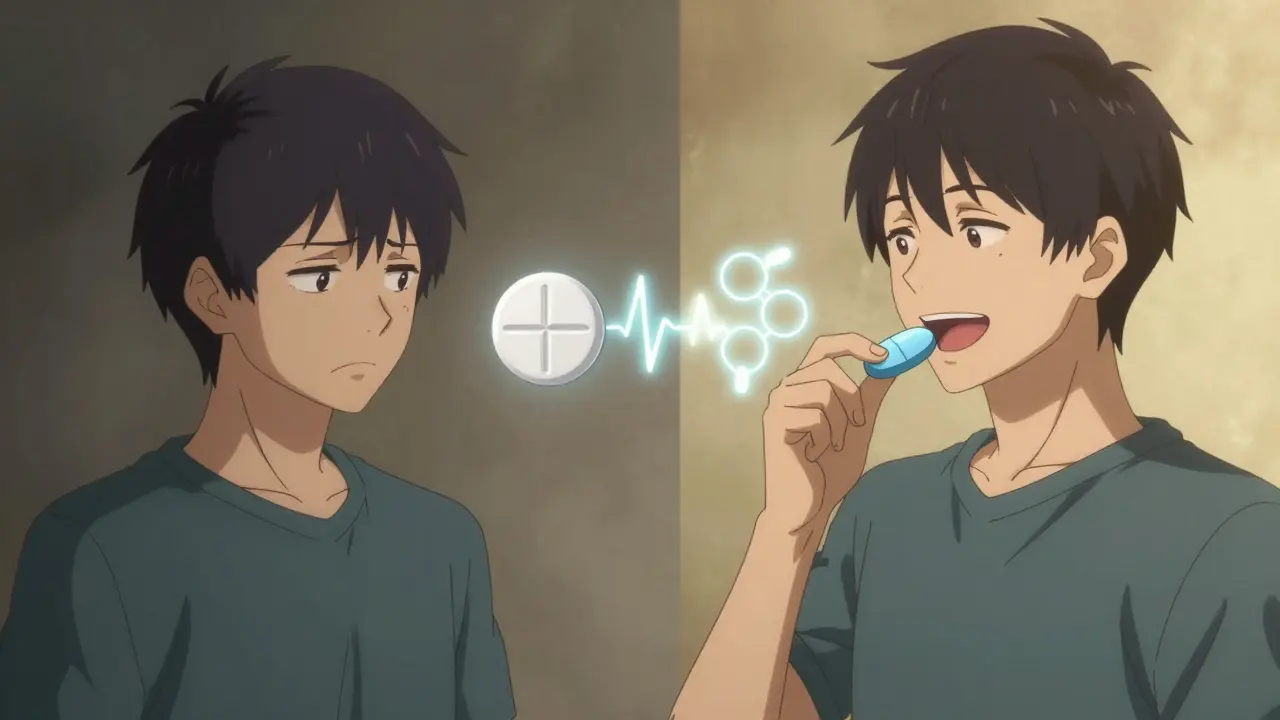
Think about it: if you’ve been taking a blue oval pill for years, and suddenly you’re handed a white circle with a weird logo, it’s natural to wonder if something’s off. That’s not just psychology-it’s real. Traditional generics often change the shape, color, or inactive ingredients to avoid patent issues. Those changes don’t affect how the drug works, but they can affect how patients feel.
A 2018 study tracking 210,000 patients found that 28.7% of people who switched to a regular generic went back to the brand-name version. That’s almost one in three. But for those who switched to an authorized generic? Only 22.3% went back. That’s a 22% drop in switchbacks. Why? Because the pill looked the same. Tasted the same. Took the same amount of time to kick in. It felt like the same drug.
Consumer Reports did a blind test with 1,200 people. They gave them unlabeled pills-brand, authorized generic, and traditional generic. Most couldn’t tell the difference between the brand and the authorized generic. But nearly half could tell the difference between the brand and the traditional generic. That’s not magic. That’s identical manufacturing.
Price still wins-but not always
Here’s the catch: authorized generics aren’t the cheapest option. They’re usually 15-25% more expensive than traditional generics after the first six months. Why? Because the brand company still has to make a profit. And they’re not trying to compete on price-they’re competing on trust.
When a new generic hits the market, the first 180 days are critical. That’s when the first generic manufacturer gets exclusive rights to sell. But here’s the twist: the brand company can launch its own authorized generic during that window. Suddenly, there are two generics on the shelf-one from a competitor, one from the brand. The competitor’s price drops. The authorized generic’s price drops too. But it still costs more than the traditional generic.
So what do patients do? When money isn’t tight, many stick with the authorized generic. They’ve had bad experiences with traditional generics. They don’t want to risk it. But when insurance pushes for the lowest-cost option, or when the patient is paying out-of-pocket, the traditional generic wins. Data shows that after the exclusivity period ends, traditional generics capture 65-75% of the market. Price wins. But only after trust has been built.
Who’s really deciding what you get?
Here’s the uncomfortable truth: you probably didn’t choose your generic. Your insurance plan did.
According to a 2022 KFF analysis, 82% of commercial insurance plans automatically switch you to any generic-authorized or not-unless your doctor writes "do not substitute." That means if your plan has a deal with a pharmacy benefit manager (PBM), and they’ve negotiated the lowest price on a traditional generic, that’s what you’ll get-even if the authorized generic is better for you.
Pharmacists know this. They’re trained to explain the difference. But most patients don’t ask. They just take what’s handed to them. A 2022 American Pharmacists Association guideline says pharmacists should proactively explain authorized generics, especially for patients with chronic conditions like epilepsy, thyroid disease, or depression, where small differences matter. But in a busy pharmacy, that doesn’t always happen.
And here’s another layer: some patients don’t even know they’re getting an authorized generic. The label doesn’t say "authorized." It just says "generic." The only way to know is to check the FDA’s Orange Book-or ask your pharmacist directly.
The hidden strategy behind authorized generics
Why do big drug companies bother making authorized generics? It’s not about helping patients. It’s about protecting profits.
The Hatch-Waxman Act of 1984 was supposed to speed up generic competition. But brand companies found a loophole: if they launch their own authorized generic, they can scare off competitors. Why? Because if a generic manufacturer knows the brand will undercut them with an identical product, they might delay entering the market. That’s exactly what the Federal Trade Commission warned about in 2011.
Some deals between brand companies and generic manufacturers include secret agreements: "We won’t launch our generic if you don’t launch your authorized generic." These are called "pay-for-delay" settlements. The FTC has tracked 23 of them between 2021 and 2022. They’re legal-but they’re not fair.
Still, for patients, the result is often good: prices drop faster. More options appear sooner. The 2022 Drug Patent Watch study on entacapone showed authorized generics drove down Medicaid prices by over 10% and retail prices by nearly 20%. That’s real savings. Just not always the kind you expect.

What patients really say
Go to Reddit’s r/pharmacy and ask: "Authorized generic vs regular generic-any difference?" You’ll get 87 responses. Sixty-three percent say they noticed no difference. Twenty-eight percent say they felt the same with traditional generics. Only 9% say they had issues with authorized generics.
One person wrote: "I take a brand-name antidepressant. My pharmacy switched me to the authorized generic. I didn’t feel anything different. My doctor didn’t even know I’d switched. I kept taking it because it worked the same." Another: "I switched to a regular generic and had stomach pain for two weeks. Went back to the brand. Then my insurance forced me to the authorized generic. Same as the brand. No pain. I’ve been on it for a year." These aren’t outliers. They’re the norm.
Is this the future of generic drugs?
Authorized generics now make up about 12% of all generic drug units dispensed in the U.S.-up from 8% in 2015. By 2028, experts predict they’ll hit 15-18%. Why? Because drug companies keep using them. And patients keep choosing them.
They’re not perfect. They’re not the cheapest. They’re not always available. But for patients who’ve been burned by traditional generics, they’re the safest bet. They’re the closest thing to the brand without the brand price tag.
The real question isn’t whether patients choose authorized generics. It’s whether the system lets them. Right now, most don’t get a choice. Insurance rules. Pharmacy contracts. Price tags. Not patient experience. Not trust. Not peace of mind.
If you’re on a chronic medication and you’ve had bad experiences with generics, ask your doctor to write "dispense as written" or "brand necessary" on your prescription. Then ask your pharmacist: "Is this an authorized generic?" If they don’t know, ask them to check the FDA’s "Products with No Applicant" list. It’s not hard. And it might make all the difference.
What you can do next
- If you’re on a long-term medication and you’ve switched to a generic, keep track of how you feel. Any new side effects? Worse symptoms? That’s a signal.
- Ask your pharmacist: "Is this an authorized generic?" If they say no, ask if one is available.
- If your insurance won’t cover the authorized generic, ask your doctor to submit a prior authorization request-explain you had issues with traditional generics.
- Check the FDA’s Orange Book or "Products with No Applicant" list online. You can search by drug name and see who makes what.
- Don’t assume all generics are the same. Authorized ones are made by the brand company. Traditional ones are made by someone else.
It’s not about being loyal to a brand. It’s about knowing what you’re taking-and having the power to choose what works for your body.





Comments (8)