When you're on rifampin for tuberculosis or another infection, your birth control might not be working like you think. It's not a myth. It's not a rumor. It's science - and it's happened to real women. Rifampin, a powerful antibiotic, can make hormonal contraceptives like the pill, patch, or ring fail - even if you take them perfectly on time. The result? Breakthrough ovulation - meaning your body releases an egg when it shouldn't - and that can lead to pregnancy.
How Rifampin Breaks Down Birth Control
Rifampin doesn't just kill bacteria. It also tricks your liver into speeding up the breakdown of hormones. Specifically, it turns on enzymes called cytochrome P450, especially CYP3A4. These enzymes are normally busy cleaning up toxins and old hormones. But when rifampin wakes them up, they start chewing through estrogen and progestin - the two key hormones in most birth control - before your body can use them. Studies show this isn't theoretical. In five well-designed studies, women taking rifampin along with combined oral contraceptives saw their estrogen levels drop by 42% to 66%. Progestin levels? Down by 30% to 83%. That's not a small change. That's enough to stop ovulation suppression. One study found that two out of four women on this combo started ovulating again - even though they were taking their pill every day. This isn't just about feeling different. It's about your body doing something it shouldn't: releasing an egg. And if you're having sex? That egg can get fertilized.Why Rifampin Is the Only Antibiotic That Does This
You've probably heard that antibiotics can mess with birth control. That's mostly wrong. Penicillin? Azithromycin? Tetracycline? None of them do this. The evidence is clear: rifampin is the only antibiotic with solid, repeated proof of reducing contraceptive hormone levels. The American Academy of Family Physicians says it plainly: "Rifampin is the only antibiotic that has been shown to reduce plasma estrogen concentrations." The Journal of the Society of Obstetricians and Gynaecologists of Canada goes even further: "When taking rifampin, oral contraceptives cannot be relied upon for contraception." Other antibiotics might cause nausea or diarrhea - which could lead to missed pills - but they don't chemically destroy your hormones. Rifampin does. That's why doctors don't warn you about amoxicillin, but they absolutely warn you about rifampin.Rifabutin: The Close Cousin That Might Be Safer
Rifabutin, another drug in the same family as rifampin, is sometimes used instead for TB treatment - especially if rifampin causes too many side effects. The good news? Rifabutin doesn't seem to have the same strong effect on birth control. In studies, women taking rifabutin with hormonal contraceptives didn't show ovulation. Their hormone levels stayed within safe ranges. That doesn't mean it's 100% safe - there's still a small risk - but it's much lower than with rifampin. If you're on rifabutin and on birth control, talk to your doctor. You might not need a backup method. But don't assume. Always check.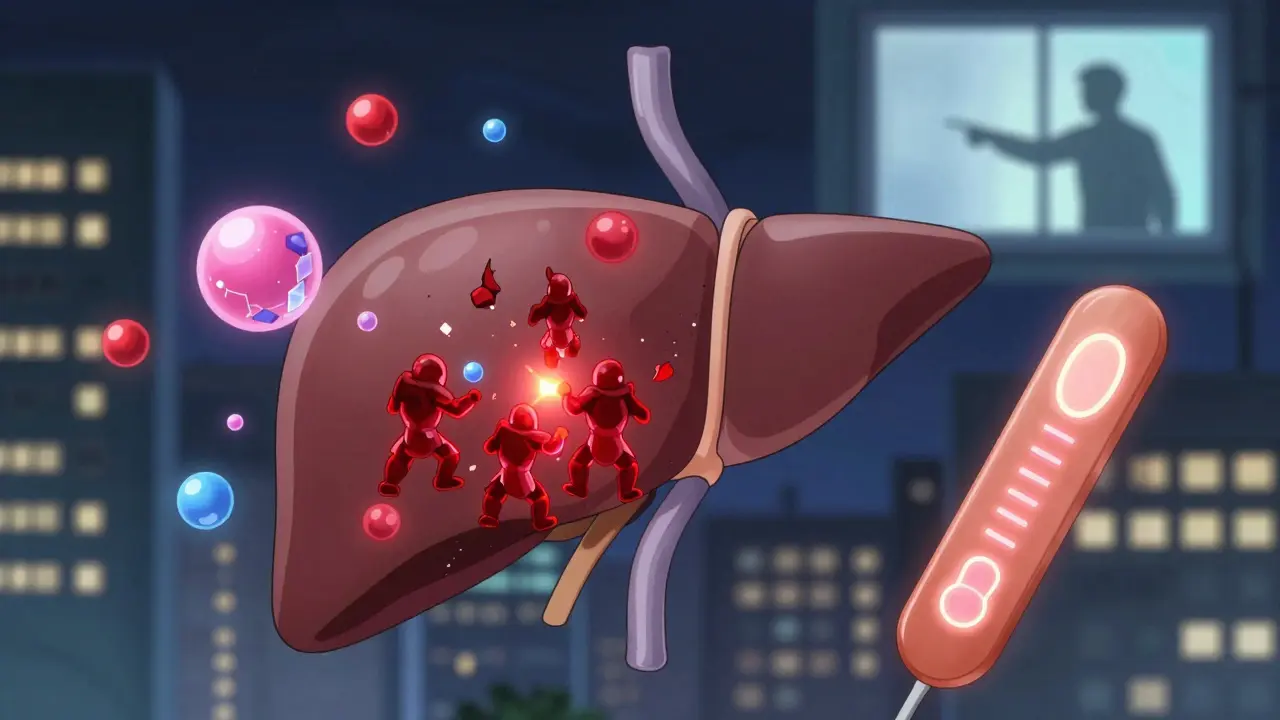
What Happens When You Get Pregnant on Birth Control and Rifampin
It's rare - but it happens. The CDC estimates that without any drugs, the pill fails about 0.3% of the time with perfect use. With rifampin? That number jumps. No one knows exactly how high - because it depends on your body, your dose, and how long you've been on both drugs. But case reports tell the story. One woman on Reddit shared: "I was on Ortho Tri-Cyclen while taking rifampin for TB treatment and got pregnant despite perfect pill adherence. My OB/GYN confirmed it was almost certainly the rifampin interaction." Another nurse with 15 years of experience said she's never seen a birth control failure from any antibiotic except rifampin or rifabutin. The UK's Committee on Safety of Medicines logged 150 cases of contraceptive failure linked to antibiotics between 1970 and 1999 - and rifampin was the common thread in the most serious ones. This isn't about being careless. It's about a hidden interaction that even some doctors forget to mention.What You Should Do If You're Taking Rifampin
Here's what the CDC, WHO, and major medical groups agree on:- Use a backup method - like condoms - for the entire time you're taking rifampin.
- Keep using backup contraception for at least 28 days after you stop rifampin. Why? Because the enzyme-inducing effect doesn't vanish the day you stop the drug. It takes weeks for your liver to calm down.
- Don't rely on higher-dose pills. Some doctors used to suggest switching to a pill with 50 mcg of estrogen. But there's no solid proof this works. It might help a little - but it's not a guarantee.
- Consider switching to a non-hormonal method. A copper IUD doesn't care about liver enzymes. A progestin implant (like Nexplanon) is also less affected - though even that needs monitoring.





Comments (14)