SSRI-NSAID GI Bleeding Risk Calculator
Assess Your Risk
Your Risk Assessment
Your risk is times higher than baseline when combining these medications.
For comparison: The average person taking an SSRI and NSAID together has a 75% higher risk of bleeding than those taking only one medication.
Key finding: Your risk is highest with non-selective NSAIDs like naproxen and diclofenac, and lowest with celecoxib.
Recommended Actions
Critical Warning Signs
- Black, tarry stools (melena)
- Vomiting blood or coffee-ground material
- Sudden dizziness or weakness
- Severe abdominal pain
Every year, millions of people take SSRIs for depression or anxiety, and just as many reach for NSAIDs for back pain, arthritis, or headaches. On their own, both are common, generally safe medications. But when taken together, they create a hidden danger that many patients - and even doctors - don’t fully understand: a sharply increased risk of upper GI bleeding.
Why This Combination Is Riskier Than You Think
SSRIs like sertraline, fluoxetine, and citalopram work by boosting serotonin in the brain. But serotonin also plays a key role in blood clotting. Platelets need serotonin to stick together and seal off damaged blood vessels. When SSRIs block serotonin reuptake into platelets, they weaken this first-line defense. Even if you’re not bleeding right now, your body’s ability to stop a small tear in your stomach lining is compromised. NSAIDs - including ibuprofen, naproxen, and diclofenac - work differently but just as dangerously. They shut down COX-1 enzymes, which are responsible for making prostaglandins. These chemicals protect your stomach by boosting mucus, reducing acid, and keeping blood flowing to the stomach lining. Without them, your stomach becomes vulnerable to damage from its own acid. Put them together, and you’re not just adding two risks. You’re multiplying them. A 2022 analysis of 10 major studies found that people taking both an SSRI and an NSAID have a 75% higher chance of upper GI bleeding than those taking just one. That’s not a small bump - it’s a major jump. The risk is even higher if you’re over 65, have had an ulcer before, or are also on blood thinners.Not All SSRIs or NSAIDs Are Created Equal
The risk isn’t the same across every drug in these classes. Some SSRIs may carry slightly more bleeding risk than others, though the difference is small. Fluvoxamine and paroxetine might be a bit more likely to interfere with platelets than escitalopram, but the evidence isn’t strong enough to say one SSRI is “safe” while another isn’t. NSAIDs vary much more. Non-selective ones like naproxen and diclofenac are the worst offenders. They hit COX-1 hard and cause more damage. Ibuprofen is the least harmful among them, but it’s still risky when paired with an SSRI. That’s where celecoxib (Celebrex) comes in. It’s a COX-2 inhibitor, meaning it mostly spares the stomach-protecting COX-1 enzyme. Studies show celecoxib has a GI bleeding risk close to baseline - only about 16% higher than not taking any NSAID at all. For someone who needs an NSAID long-term and is also on an SSRI, celecoxib is often the best choice.What Doctors Should Do - But Often Don’t
Here’s the problem: most doctors don’t routinely check for this interaction. A 2021 survey of over 1,200 primary care providers found that only 39% asked patients if they were taking NSAIDs before prescribing an SSRI. Only 22% prescribed a protective medication like a proton pump inhibitor (PPI) when both were needed. Patients aren’t being warned either. In a 2022 survey, 68% of people who took both an SSRI and an NSAID said they were never told about the bleeding risk. That’s unacceptable. This isn’t a rare side effect - it’s a well-documented, preventable danger. The American College of Gastroenterology and other major groups have been clear since 2021: if you’re going to prescribe both, you must also prescribe a PPI. Omeprazole 20mg daily is the standard. It cuts the excess bleeding risk from the combo by about 70%. That’s not a minor benefit - it’s the difference between a 1 in 20 chance of bleeding and a 1 in 70 chance.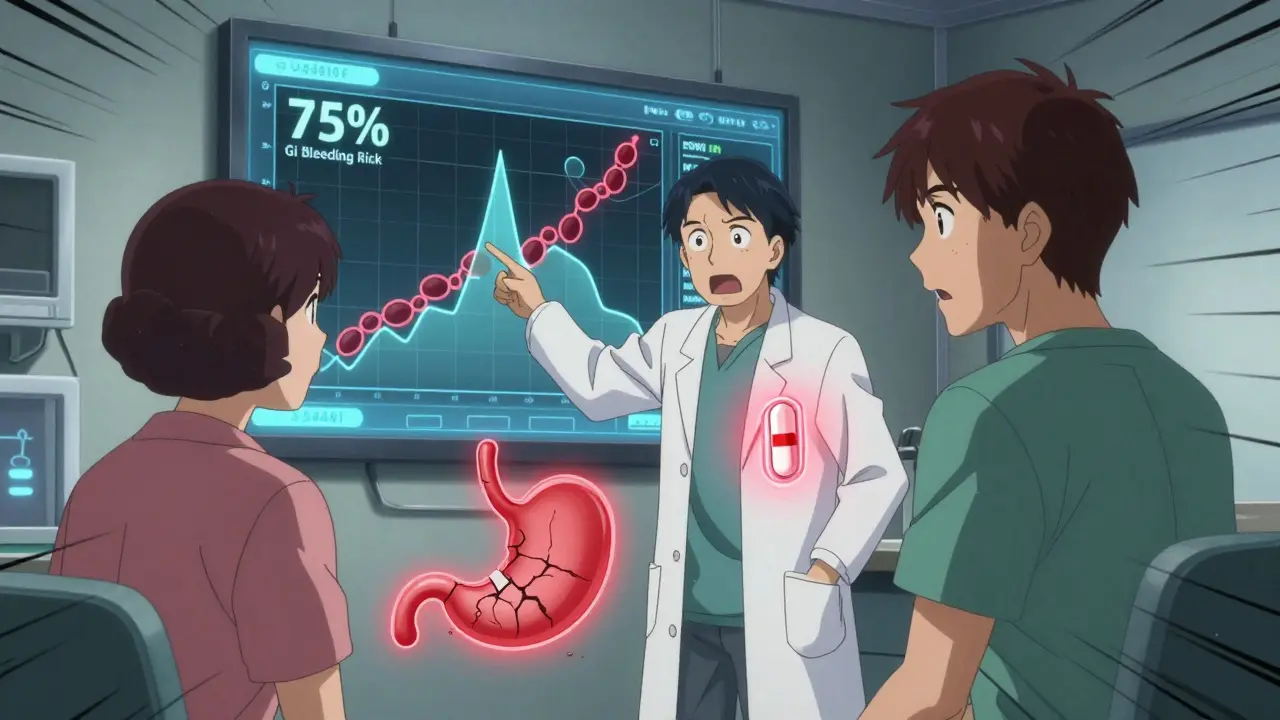
What You Can Do Right Now
If you’re taking an SSRI and an NSAID together, here’s what to do:- Don’t stop either medication without talking to your doctor. Abruptly stopping an SSRI can cause withdrawal. Stopping an NSAID cold turkey might make your pain worse.
- Ask if you really need both. Can your pain be managed with acetaminophen (Tylenol)? It doesn’t affect platelets or stomach lining. For many people, it’s a safer alternative to NSAIDs.
- Ask if you can switch NSAIDs. If you’re on naproxen or diclofenac, ask about switching to ibuprofen - or better yet, celecoxib.
- Ask if you need a PPI. If you’re over 60, have had a stomach ulcer, or take aspirin or blood thinners, you should be on a PPI. If you’re not, ask why.
- Know the warning signs. Black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden dizziness or weakness; or severe abdominal pain are all red flags. Don’t wait - go to the ER.
Real Stories, Real Consequences
Online forums are full of stories that show how this plays out in real life. One Reddit user described black, sticky stools for three days before ending up in the ER. Another shared how they’d been on sertraline and ibuprofen for years without issues - until they didn’t. They ended up hospitalized with a bleeding ulcer. But there are also success stories. One patient with rheumatoid arthritis and depression switched from naproxen to celecoxib and started taking omeprazole daily. She’s been symptom-free for over a year. Her story proves this risk can be managed - but only if you act.
What’s Changing in 2025
Health systems are finally catching up. Since 2019, major hospitals like Cleveland Clinic and Mayo Clinic have added automated alerts in their electronic records when a doctor tries to prescribe an SSRI and NSAID together. After Cleveland Clinic rolled out the alert, upper GI bleeding admissions dropped by 42% among patients on both drugs. New tools are coming. Researchers are now using AI to predict who’s most at risk by analyzing age, medical history, lab results, and even genetic markers like CYP2C19 - which affects how your body processes both SSRIs and PPIs. A 2023 study showed this AI model could predict bleeding risk with 86% accuracy. Pharmaceutical companies are also working on new formulations. One dual-release pill combines ibuprofen with omeprazole in a single tablet. It’s in late-stage trials and could be available soon. That means fewer pills to remember - and better protection built right in.Bottom Line: This Is Preventable
SSRIs and NSAIDs are both essential tools in modern medicine. But when used together without protection, they’re a dangerous pair. The science is clear. The guidelines are clear. The tools to prevent harm exist. If you’re on both, talk to your doctor today. Ask: Do I need both? Is there a safer alternative? Should I be on a PPI? Don’t assume it’s fine because you’ve taken them for months or years. Bleeding doesn’t always come with warning signs - and once it starts, it can be life-threatening. This isn’t about fear. It’s about awareness. And awareness saves lives.Can I take ibuprofen with an SSRI safely?
Taking ibuprofen with an SSRI increases your risk of upper GI bleeding by about 75%. While ibuprofen is the least risky NSAID, it’s still dangerous when combined with an SSRI. If you need pain relief and are on an SSRI, talk to your doctor about switching to acetaminophen (Tylenol) or adding a proton pump inhibitor like omeprazole. Never take them together without protection.
Is celecoxib safer than other NSAIDs when taking an SSRI?
Yes. Celecoxib (Celebrex) is a COX-2 selective NSAID that doesn’t interfere much with stomach-protecting prostaglandins. Studies show its GI bleeding risk is close to baseline - only about 16% higher than not taking an NSAID at all. When paired with an SSRI, it’s significantly safer than naproxen, diclofenac, or even ibuprofen. For long-term pain management with an SSRI, celecoxib is often the preferred NSAID option.
Do all SSRIs carry the same bleeding risk?
Most SSRIs work the same way - by blocking serotonin reuptake in platelets - so their bleeding risk is generally similar. Some studies suggest escitalopram might have a slightly lower risk than fluvoxamine or paroxetine, but the difference isn’t large enough to base a switch on alone. The bigger issue is the combination with NSAIDs, not which SSRI you’re on. Focus on reducing NSAID risk first.
Should I take a PPI if I’m on an SSRI and NSAID?
Yes - if you’re taking both, you should be on a proton pump inhibitor (PPI) like omeprazole 20mg daily. Studies show PPIs reduce the excess bleeding risk from this combination by about 70%. This is standard of care according to the American College of Gastroenterology. If your doctor hasn’t prescribed one, ask why. It’s not optional for high-risk patients.
What are the signs of GI bleeding from this interaction?
Watch for black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, weakness, rapid heartbeat, or severe stomach pain. These are signs of active bleeding. Don’t wait to see if it gets better - go to the emergency room immediately. GI bleeding can be silent until it’s severe.
Can I switch to a different antidepressant to avoid this risk?
Yes. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelets or serotonin reuptake, so it doesn’t increase bleeding risk. If you’re on an SSRI and need long-term NSAID use, switching to bupropion could eliminate the interaction. Talk to your doctor about whether this is a good option for your depression or anxiety symptoms.
How common is this dangerous combination?
Very. In the U.S., about 34.7 million adults take antidepressants, and 76.5% of those are SSRIs. Meanwhile, 17 million Americans use NSAIDs daily. A 2022 audit found that nearly 28% of SSRI users were also prescribed an NSAID within six months - that’s over 9.8 million people at increased risk. Most don’t know the danger.
Are there tests to check my personal risk?
Yes. Your doctor can use the ACG Upper GI Risk Calculator, which considers age, prior ulcer history, H. pylori infection, and other factors. Genetic testing for CYP2C19 mutations can also help - it affects how you process both SSRIs and PPIs. If you’re high-risk, your doctor may recommend testing for H. pylori and treating it before starting both medications.



Comments (14)