GI Bleeding Risk Calculator
Personalized Risk Assessment
This calculator estimates your risk of gastrointestinal bleeding when taking SSRIs and NSAIDs together based on your specific circumstances.
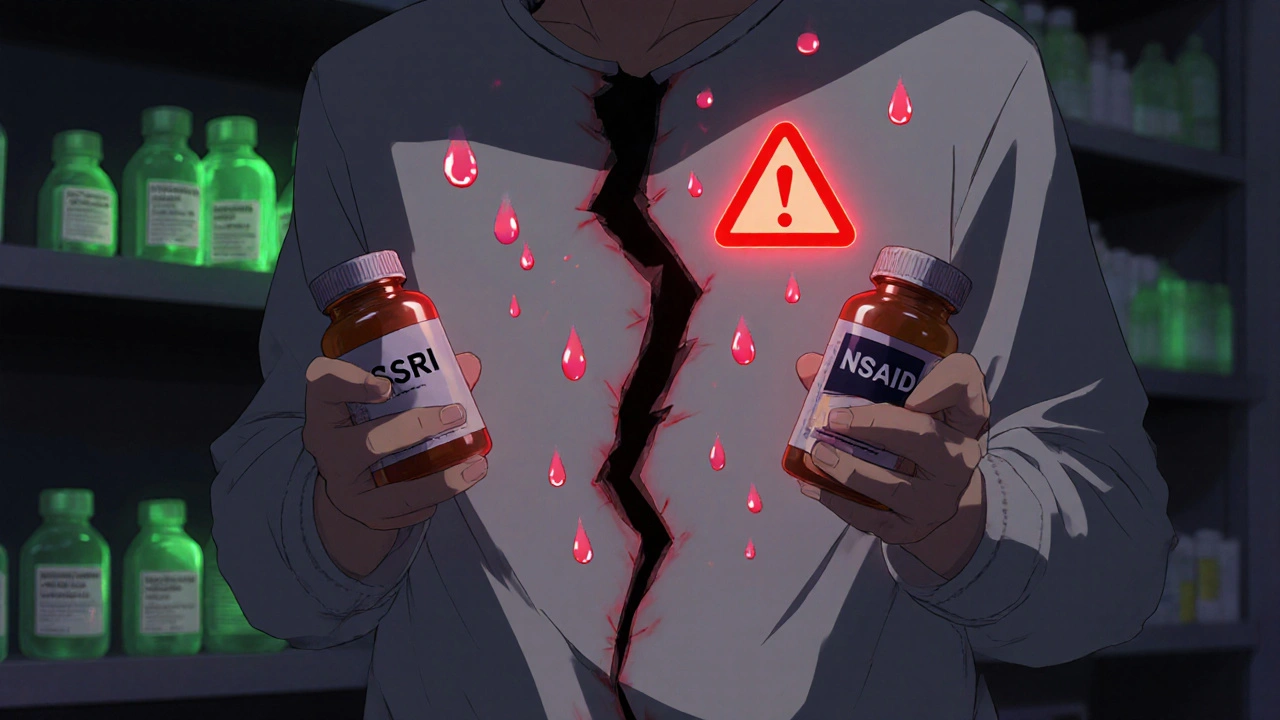
When you’re taking an SSRI for depression or anxiety, and you also need pain relief for arthritis or a bad back, it’s easy to reach for an over-the-counter NSAID like ibuprofen or naproxen. But here’s something most people don’t know: combining SSRIs with NSAIDs can dramatically increase your risk of serious stomach bleeding. This isn’t a rare side effect - it’s a well-documented, dangerous interaction that’s happening far more often than doctors and patients realize.
Why This Combination Is So Dangerous
SSRIs - drugs like sertraline, fluoxetine, and escitalopram - work by increasing serotonin in the brain. But serotonin isn’t just a mood chemical. It’s also critical for blood clotting. Platelets need serotonin to stick together and stop bleeding. SSRIs block the serotonin transporter on platelets, which means they can’t clump effectively when you get a cut or irritation in your stomach lining. NSAIDs like ibuprofen, naproxen, and diclofenac do something different but equally harmful to your stomach. They block enzymes that make protective mucus and reduce blood flow to the stomach lining. This makes your stomach more vulnerable to acid damage. When you take both together, you get a one-two punch: your stomach lining gets damaged, and your body can’t clot properly to stop the bleeding. A 2022 meta-analysis in Nature Scientific Reports reviewed data from over 1.2 million patients and found that using SSRIs and NSAIDs together increases the risk of upper GI bleeding by 75% compared to using NSAIDs alone. That’s not a small increase. It’s the same level of risk as taking warfarin, a blood thinner prescribed for heart conditions.Who’s at the Highest Risk?
Not everyone who takes this combo will bleed. But some people are far more vulnerable:- People over 65 - aging stomachs produce less protective mucus
- Those with a history of ulcers or GI bleeding - even if it was years ago
- People taking low-dose aspirin - adding aspirin to SSRIs and NSAIDs can push bleeding risk over 12 times higher
- Those on multiple blood-thinning medications - like clopidogrel or apixaban
- Patients taking high-dose NSAIDs - over 1,200 mg of ibuprofen per day
- People who’ve been on SSRIs for more than 90 days - risk increases with duration
Not All NSAIDs Are the Same
If you need pain relief while on an SSRI, not all NSAIDs carry the same risk. Some are worse than others:- Worst offenders: Naproxen, diclofenac - highest bleeding risk
- Medium risk: Ibuprofen - lower than naproxen, but still dangerous with SSRIs
- Lowest risk NSAID: Celecoxib (Celebrex) - a COX-2 inhibitor that’s gentler on the stomach
The Safer Alternative: Acetaminophen
Here’s the good news: there’s a much safer option for pain relief if you’re on an SSRI. Acetaminophen (paracetamol) - the active ingredient in Tylenol - doesn’t affect platelets or stomach lining. It doesn’t interfere with serotonin or prostaglandins. A 2023 meta-analysis in Digestive Diseases and Sciences confirmed that acetaminophen has no increased bleeding risk when taken with SSRIs. Many patients don’t know this. On patient forums like Reddit and Drugs.com, nearly 70% of users said they were never warned about the danger. One user wrote: “I was on sertraline and ibuprofen for six months. Then I ended up in the ER with internal bleeding. No one ever told me this could happen.” Switching from ibuprofen to acetaminophen isn’t just safer - it’s often just as effective for common aches like headaches, back pain, or joint discomfort. For chronic pain, physical therapy, heat wraps, or even low-dose gabapentin might be better long-term options than NSAIDs.What Doctors Should Do - and Often Don’t
The American Gastroenterological Association (AGA) has clear guidelines: if you must take both an SSRI and an NSAID, you need a proton pump inhibitor (PPI) like omeprazole or pantoprazole. PPIs reduce stomach acid and help heal the lining, cutting bleeding risk by about 70%. Yet, a 2021 study in JAMA Internal Medicine found that in 12 primary care clinics, 28% of patients on both drugs were not prescribed a PPI. That’s nearly 3 out of 10 people being put at unnecessary risk. Doctors often miss this because:- Patients don’t mention OTC NSAIDs - they think “it’s just ibuprofen, it’s harmless”
- Prescribing systems don’t flag the interaction
- Many physicians assume the risk is too low to worry about
Real Solutions: What You Can Do Today
If you’re on an SSRI and regularly take NSAIDs, here’s what to do:- Stop NSAIDs if possible. Try acetaminophen first. For mild pain, it’s usually enough.
- If you must use an NSAID, use the lowest effective dose for the shortest time. Avoid daily use unless absolutely necessary.
- Ask your doctor about a PPI. Omeprazole 20 mg once daily is inexpensive and widely available. It’s not a cure-all, but it cuts your risk dramatically.
- Know the warning signs. Black, tarry stools; vomiting blood; sudden dizziness or weakness; unexplained fatigue - these could mean internal bleeding. Don’t wait. Go to the ER.
- Review all your meds with your pharmacist. Many OTC cold pills, menstrual pain relievers, and topical creams contain NSAIDs. Check labels.

The Bigger Picture
This isn’t just about one drug combo. It’s about how we treat chronic pain and depression in modern medicine. Millions of people take SSRIs. Nearly one in five adults in the U.S. uses NSAIDs regularly. That’s tens of millions of potential interactions. Between 2018 and 2022, prescriptions for acetaminophen among SSRI users rose by 18%, while NSAID use dropped by 12%. That’s progress. But it’s still not enough. New tools are emerging. In 2023, Epic EHR systems rolled out a GI-BLEED risk calculator that factors in your age, medications, genetics, and history to give you a personalized risk score. It’s accurate 89% of the time. Some new antidepressants - like vortioxetine - are showing promise with lower bleeding risk. But they’re not widely available yet. For now, the safest choice is simple: if you’re on an SSRI, treat pain with acetaminophen. If you need more, talk to your doctor before reaching for that bottle of ibuprofen.What If You’ve Already Had Bleeding?
If you’ve had a GI bleed while on an SSRI and NSAID, your doctor should reassess everything. You’ll likely need to:- Stop the NSAID permanently
- Stay on a PPI long-term
- Consider switching to an SSRI with lower platelet effects - like sertraline or citalopram - instead of fluoxetine or paroxetine
- Get screened for H. pylori infection, which also increases bleeding risk
Can I take ibuprofen with sertraline?
Taking ibuprofen with sertraline increases your risk of stomach bleeding by about 75% compared to using ibuprofen alone. It’s not impossible, but it’s dangerous. If you need pain relief, switch to acetaminophen (Tylenol) instead. If you must use ibuprofen, ask your doctor about taking a proton pump inhibitor like omeprazole at the same time to protect your stomach.
Which antidepressants have the lowest bleeding risk?
SSRIs vary in how strongly they affect platelets. Sertraline and citalopram have weaker effects on serotonin reuptake in platelets, making them lower risk than fluoxetine or paroxetine. However, all SSRIs carry some bleeding risk when combined with NSAIDs. The safest approach is to avoid NSAIDs altogether, regardless of which SSRI you’re on.
Does every person on SSRIs and NSAIDs get GI bleeding?
No. Most people won’t have a major bleed. But the risk is real and unpredictable. Studies show the annual risk of serious GI bleeding is about 1.5% for people on both drugs - that’s 1 in 67 people each year. For someone over 65 with a past ulcer, the risk jumps to over 5%. Even a small chance of life-threatening bleeding is too high when safer alternatives exist.
Are there any natural alternatives to NSAIDs for pain?
Yes. For mild to moderate pain, try heat therapy, physical therapy, acupuncture, or topical capsaicin cream. Turmeric and ginger have mild anti-inflammatory effects, though they’re not as strong as NSAIDs. For chronic pain, talk to your doctor about non-drug options like cognitive behavioral therapy or low-dose gabapentin - both are safer with SSRIs.
Can I take aspirin with SSRIs?
No - combining aspirin with SSRIs is especially dangerous. Aspirin thins the blood and damages the stomach lining. When you add an SSRI, you’re essentially stacking three bleeding risks: aspirin’s antiplatelet effect, SSRIs’ effect on platelet serotonin, and NSAIDs’ stomach damage. This combo has been linked to over 12 times higher bleeding risk than not taking any of them. If you’re on low-dose aspirin for heart health, talk to your doctor about alternatives like clopidogrel or lifestyle changes.



Comments (8)