Chlamydia, gonorrhea, and syphilis aren’t just old-school health warnings-they’re active, growing threats with real consequences. In 2021, the U.S. saw over 2.5 million cases of just these three bacterial STIs. Half of them were in people under 25. And while cases dropped 9% in 2024, that doesn’t mean the problem is fading-it means we’re finally getting better at catching them. But catching them isn’t enough. Knowing how to treat them, who needs testing, and how to stop them from spreading is what actually saves lives.
What You Don’t Know Can Hurt You
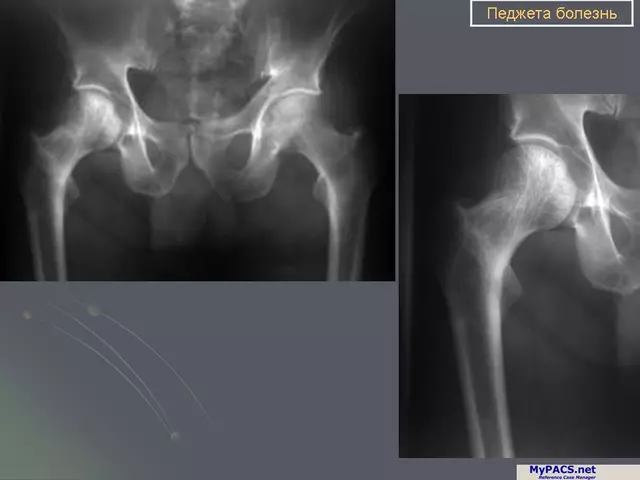
Chlamydia is the quiet killer. Up to 95% of women and half of men show no symptoms at all. You could have it for months, feel fine, and still be damaging your reproductive system. Left untreated, chlamydia can lead to pelvic inflammatory disease (PID), which scars fallopian tubes and raises the risk of ectopic pregnancy by six times. One in five women with untreated chlamydia ends up infertile. And it’s not just women. Men can develop epididymitis, a painful swelling of the tube behind the testicle that can affect fertility too. Gonorrhea acts faster. It’s more likely to cause symptoms-yellow discharge, burning when you pee, spotting between periods-but even then, nearly half of infected people don’t notice anything. The real danger? It can spread through the bloodstream. Disseminated gonococcal infection (DGI) causes joint pain, skin sores, and fever. It’s rare, but it can be life-threatening. And gonorrhea is fighting back. Antibiotic resistance is climbing. What worked five years ago might not work now. That’s why the CDC now recommends a one-two punch: ceftriaxone shot plus azithromycin pill. Even then, resistance to azithromycin is showing up in 30-50% of cases in some areas. Syphilis is the chameleon. It doesn’t just show up as one thing-it changes over time. First, a painless sore (chancre) appears where the bacteria entered, usually on the genitals, anus, or mouth. It heals on its own, so people think they’re fine. Weeks later, a rash shows up-often on the palms and soles-along with fever, swollen glands, and fatigue. That rash fades too. Then, for years, nothing. But if it’s not treated, syphilis can attack your heart, brain, and nerves. It can cause dementia, blindness, or stroke. Congenital syphilis-passed from mother to baby-is surging. In the U.S., cases jumped 273% between 2017 and 2021. That’s why every pregnant woman should be tested at least twice during pregnancy: once early and again at 28 weeks in high-risk areas.How They’re Diagnosed
You can’t guess these infections. You need tests. For chlamydia and gonorrhea, a simple urine sample works for most people. If you’ve had anal or oral sex, a swab from the rectum or throat is needed too. These tests look for the bacteria’s DNA. Fast, accurate, and non-invasive. Syphilis is different. It’s a blood test. Your body makes antibodies to fight the Treponema pallidum bacteria, and those show up in your blood. There are two types: screening tests (like RPR or VDRL) and confirmatory tests (like FTA-ABS). The screening test tells if you’ve been exposed. The confirmatory test tells if it’s active. If you’ve had syphilis before, you’ll always test positive on the confirmatory test-even after cure-so doctors look at both results together.How They’re Treated
Treatment is straightforward-if you catch it early. Chlamydia: One of two options. Either doxycycline (100 mg twice a day for 7 days) or a single 1-gram dose of azithromycin. Both work in over 95% of cases. But if you’re pregnant, azithromycin is the only safe choice. Doxycycline can harm fetal bone development. Gonorrhea: A single 500-mg shot of ceftriaxone into the muscle, plus a single 1-gram pill of azithromycin. This combo is the last reliable line of defense. If you have throat gonorrhea, you need a follow-up test in 7-14 days. Treatment fails more often there. And if you’re allergic to penicillin or ceftriaxone? There’s no good backup yet. That’s why new drugs like zoliflodacin are in phase 3 trials-with 96% cure rates-and could be approved by 2025. Syphilis: Depends on how long you’ve had it. Early syphilis (less than a year)? One shot of benzathine penicillin G (2.4 million units). Late syphilis (over a year) or unknown duration? Three shots, one per week. If you’re allergic to penicillin, alternatives exist but are less effective and require close monitoring. For pregnant women, penicillin is the only option. No exceptions.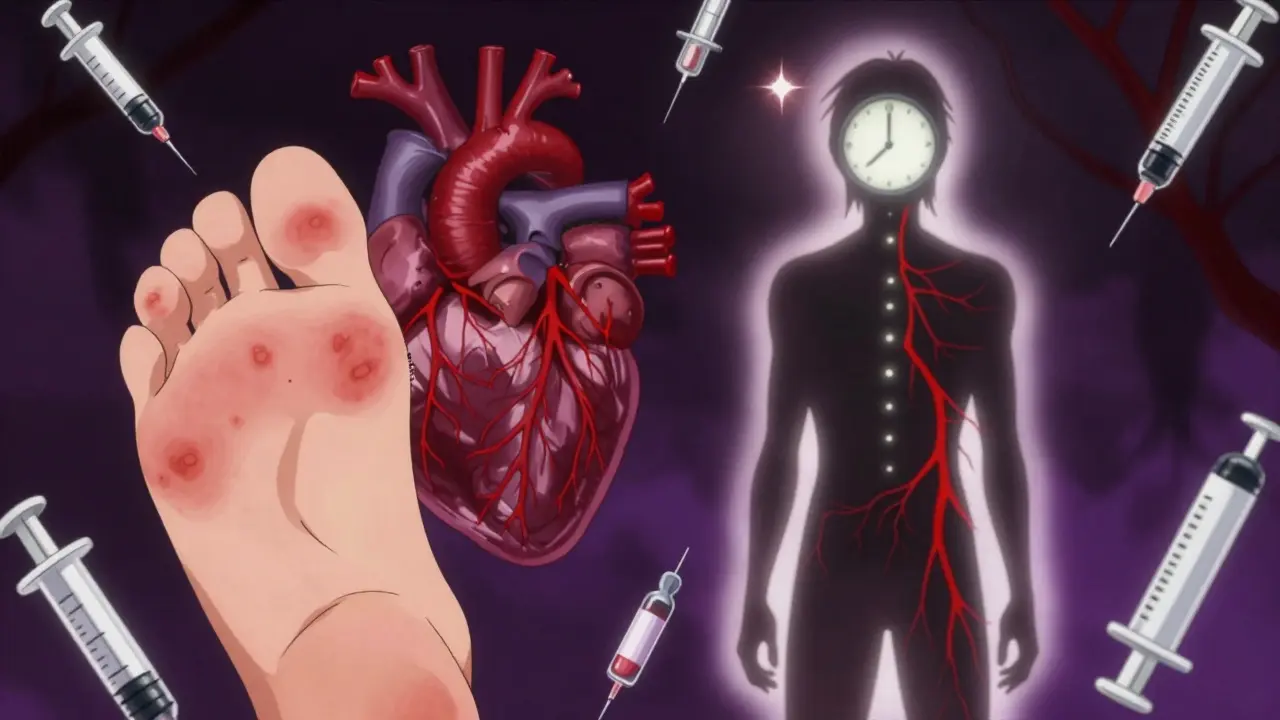
Why Partners Matter
Treating yourself isn’t enough. If your partner has it and you don’t treat them, you’ll just get it back. That’s why CDC guidelines say: anyone you had sex with in the last 60 days for chlamydia or gonorrhea needs to be treated. For syphilis, it’s the last 90 days. You don’t need to name names. Clinics offer anonymous partner notification services. You can even send a text message through a secure portal that tells them to get tested without revealing your identity. And if you’re reinfected? That’s not rare. About 1 in 5 young women get chlamydia again within a year. That’s why you need a repeat test three months after treatment-even if you feel fine and your partner was treated.The New Game-Changer: DoxyPEP
There’s a new tool: doxycycline after sex. Called DoxyPEP, it’s a single 200-mg pill taken within 72 hours of condomless sex. Three major studies showed it cuts chlamydia, gonorrhea, and syphilis rates by 47% to 73%-but only in men who have sex with men and transgender women on PrEP. It didn’t work in cisgender women. Why? We don’t fully know. Maybe differences in vaginal microbiome or exposure patterns. Right now, the CDC only recommends it for high-risk MSM and transgender women. Not because it’s unsafe for others, but because the data doesn’t support it yet. If you’re in that group and on PrEP, ask your provider about DoxyPEP. It’s not a replacement for condoms-but it’s a powerful backup.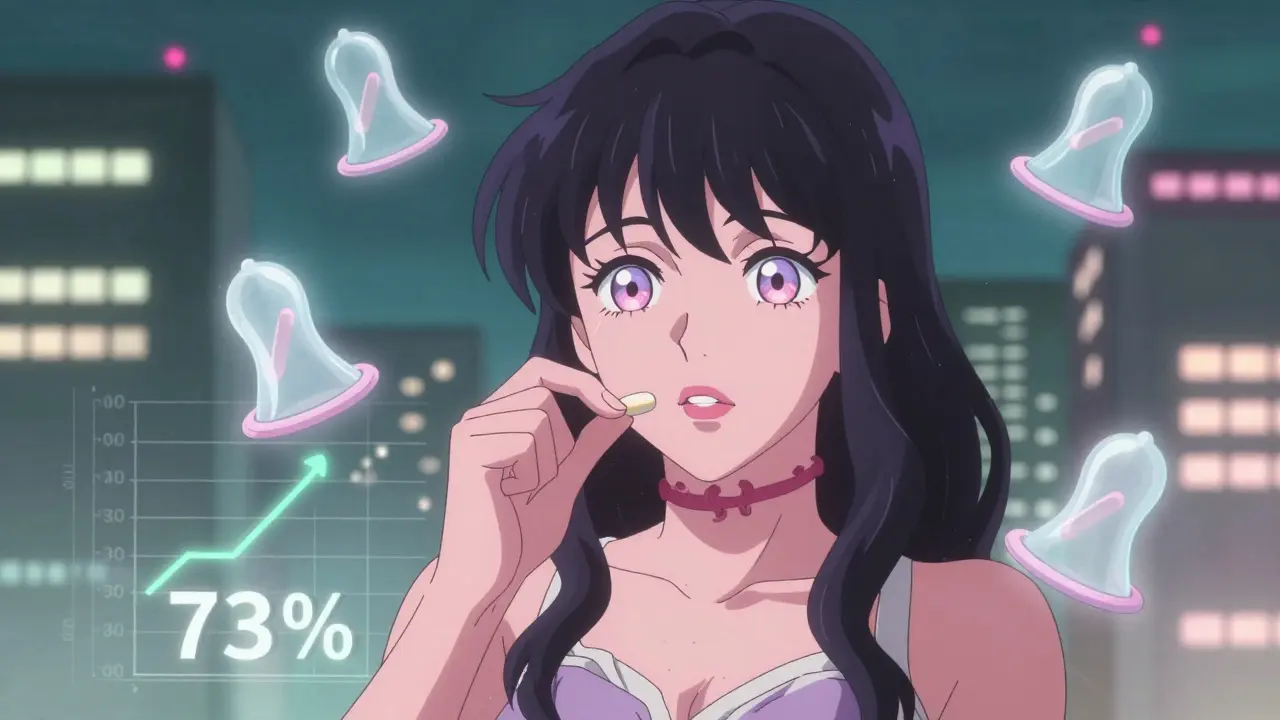
Prevention Is Still the Best Defense
Condoms reduce chlamydia and gonorrhea transmission by 60-90%. For syphilis, they cut risk by 50-70%. That’s huge. But condoms aren’t foolproof. Oral sex doesn’t always involve a condom. Anal sex often doesn’t. That’s why testing is non-negotiable. If you’re under 25 and sexually active, get tested for chlamydia and gonorrhea every year. If you have new or multiple partners, get tested every 3-6 months. If you’re pregnant, get tested at your first visit and again at 28 weeks. If you’re a man who has sex with men, get tested every 3 months for all three STIs. And if you’ve ever had an STI, get tested again after any new partner-even if you used a condom.The Bigger Picture
These infections aren’t just medical-they’re social. Black Americans face chlamydia rates 5.6 times higher than white Americans. Gonorrhea rates are 6.7 times higher. Syphilis rates are 3.5 times higher. Why? Lack of access to care, stigma, underfunded clinics, and systemic distrust in healthcare. The CDC spends $16 billion a year treating STIs in the U.S. alone. But prevention programs get a fraction of that. The WHO wants to cut syphilis in pregnant women by 90% and chlamydia/gonorrhea by 70% by 2030. That’s possible-but only if we invest in testing, treatment, education, and trust. Right now, the pipeline for new antibiotics is empty. We’re running out of options for gonorrhea. We need new drugs. We need better tests. We need more clinics. And we need to stop treating STIs like moral failures. They’re infections. They’re treatable. They’re preventable. But only if we act.What You Should Do Today
- If you’re sexually active and under 25: Get tested for chlamydia and gonorrhea now. Don’t wait for symptoms.
- If you’ve had unprotected sex in the last 72 hours and you’re a man who has sex with men or a transgender woman on PrEP: Ask your provider about DoxyPEP.
- If you’re pregnant: Make sure you’ve been tested for syphilis at your first visit and again at 28 weeks.
- If you’ve been treated for an STI: Get retested in 3 months. Reinfection is common.
- If you’ve had an STI before: Talk to your partner. Get tested together. Don’t assume they’re clean.
STIs don’t care about your age, gender, or relationship status. They only care if you’re exposed. And if you’re exposed, you need to know how to respond. Knowledge saves more than just your health-it saves your future.




Comments (12)