When you start a new medication, your doctor might say, "You might get a headache or feel nauseous." That sounds simple - but what you’re being told isn’t always accurate. Many people think all unpleasant symptoms from a drug are "side effects." But in medical terms, that’s not quite right. There’s a real difference between a side effect and an adverse drug reaction - and confusing them can lead to unnecessary fear, wrong decisions, or even dangerous outcomes.
What Exactly Is a Side Effect?
A side effect is a known, predictable reaction to a drug that happens because of how the drug works in your body. It’s not a mistake. It’s not an accident. It’s built into the drug’s biology. For example, if you take an antihistamine for allergies, you might get drowsy. That’s not a bug - it’s a feature. Antihistamines block histamine, which reduces sneezing and runny nose, but histamine also helps keep you awake. So drowsiness is a direct, expected result of the drug’s action. That’s a side effect. These are the kinds of reactions that show up in clinical trials. Researchers compare people taking the drug with people taking a placebo. If more people on the drug get nausea, dry mouth, or fatigue - and the difference is statistically significant - then it’s labeled a side effect. The FDA requires drug makers to list these in the prescribing information. Side effects are usually dose-dependent. The higher the dose, the more likely you are to feel them. Take too much acetaminophen? Your liver struggles. Take a standard dose of statins? Muscle aches might happen. These aren’t surprises. They’re part of the risk-benefit calculation your doctor made when prescribing the drug.What Is an Adverse Drug Reaction?
An adverse drug reaction (ADR) is a broader term. It includes side effects - but also other harmful responses that aren’t so predictable. The World Health Organization defines an ADR as "a response to a drug which is noxious and unintended and which occurs at doses normally used." That sounds similar, right? But here’s the key: not all ADRs are side effects. Type A reactions are the predictable ones - the side effects we just talked about. They make up about 80-85% of all ADRs. Think: diarrhea from antibiotics, low blood pressure from blood pressure meds, or constipation from opioids. Type B reactions are different. They’re unpredictable. They’re not tied to the drug’s main action. They’re rare, often serious, and sometimes life-threatening. An allergic reaction to penicillin? That’s a Type B ADR. A sudden, dangerous drop in white blood cells from a drug you’ve taken for months? That’s a Type B ADR. These don’t show up clearly in clinical trials because they’re too rare to catch before a drug hits the market. So while all side effects are ADRs, not all ADRs are side effects. Side effects are the expected, common ones. ADRs include those - plus the rare, unexpected, and sometimes dangerous ones.What’s an Adverse Event? (And Why It’s Not the Same)
Now let’s clear up the third term you’ll hear: adverse event. An adverse event is any negative health occurrence that happens after you take a drug - whether or not the drug caused it. Think of it like this: You start a new blood pressure pill. Two days later, you fall and break your wrist. Was the drug the cause? Maybe not. Maybe you were rushing to answer the phone and tripped. But because the fall happened after you started the pill, it gets logged as an adverse event. Adverse events are the raw data. They’re what patients report. What doctors note. What pharmacies send to the FDA’s MedWatch system. But they’re not proof of harm from the drug. Just coincidence. That’s why researchers dig deeper. They look at patterns. If 10,000 people take a drug and 200 get a rash - and only 50 out of 10,000 on placebo get the same rash - then it’s likely a side effect. But if 200 people on the drug and 190 on placebo get the rash? Then it’s probably not caused by the drug. It’s just an adverse event. In 2020, a study on the blood thinner apixaban found that 12.3% of patients reported headaches. So did 11.8% of people on placebo. That’s not a side effect. That’s noise. But major bleeding? That happened in 2.1% of the apixaban group and only 0.5% in the placebo group. That’s a side effect. It’s a real, confirmed risk.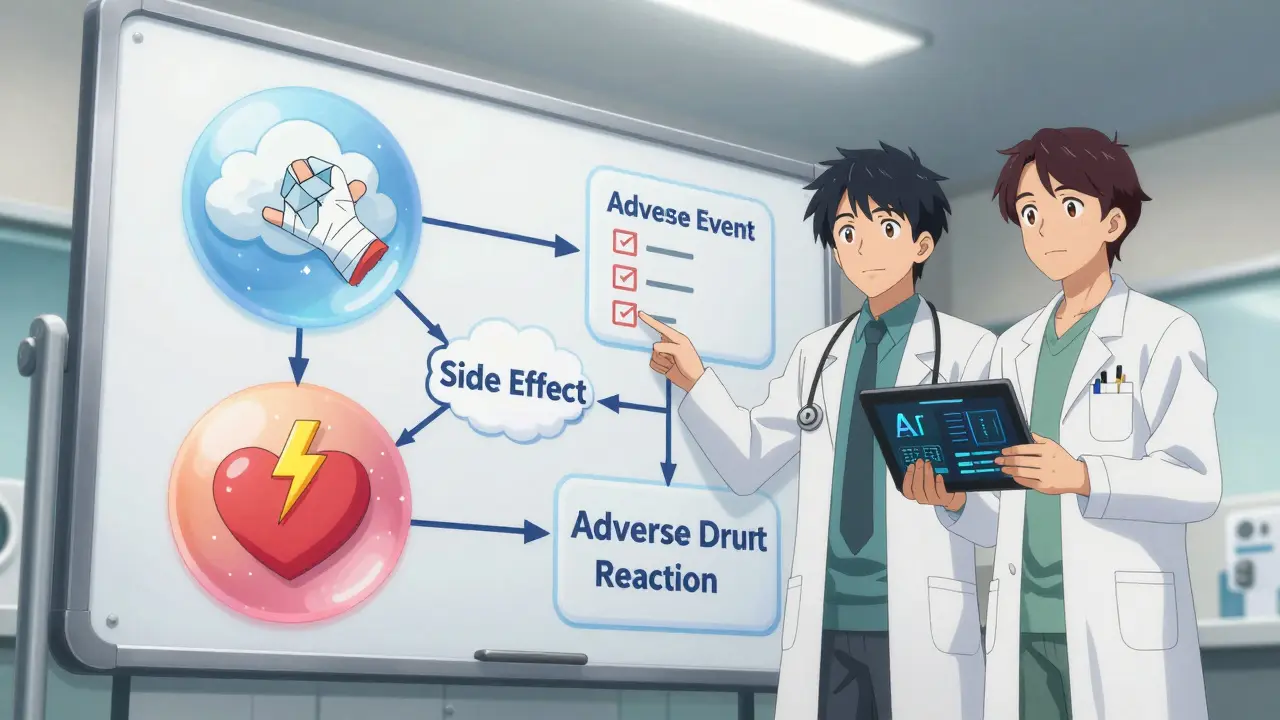
Why This Distinction Matters in Real Life
Mixing up these terms isn’t just a technical error. It has real consequences. A 2021 study found that 43% of patients stopped taking life-saving medications because they thought every bad feeling was a "side effect" - even if it wasn’t caused by the drug. Someone gets a stomachache while on statins, assumes it’s the pill, and quits. Then they have a heart attack six months later. Doctors make the same mistake. A 2021 survey by the Institute for Safe Medication Practices showed that 68% of healthcare workers use "side effect" and "adverse reaction" interchangeably in notes. That messes up safety tracking. It makes it harder to spot real dangers. It leads to wrong conclusions. The FDA and global health groups have been pushing for clearer language. Drug labels now have to separate "adverse events" (all reports) from "adverse reactions" (confirmed causes). But old habits die hard. In hospitals, teams that train staff to use the right terms have seen a 27% drop in unnecessary medication stops. Patients who understand the difference are more likely to stick with their treatment - and report real problems faster.How to Tell the Difference in Practice
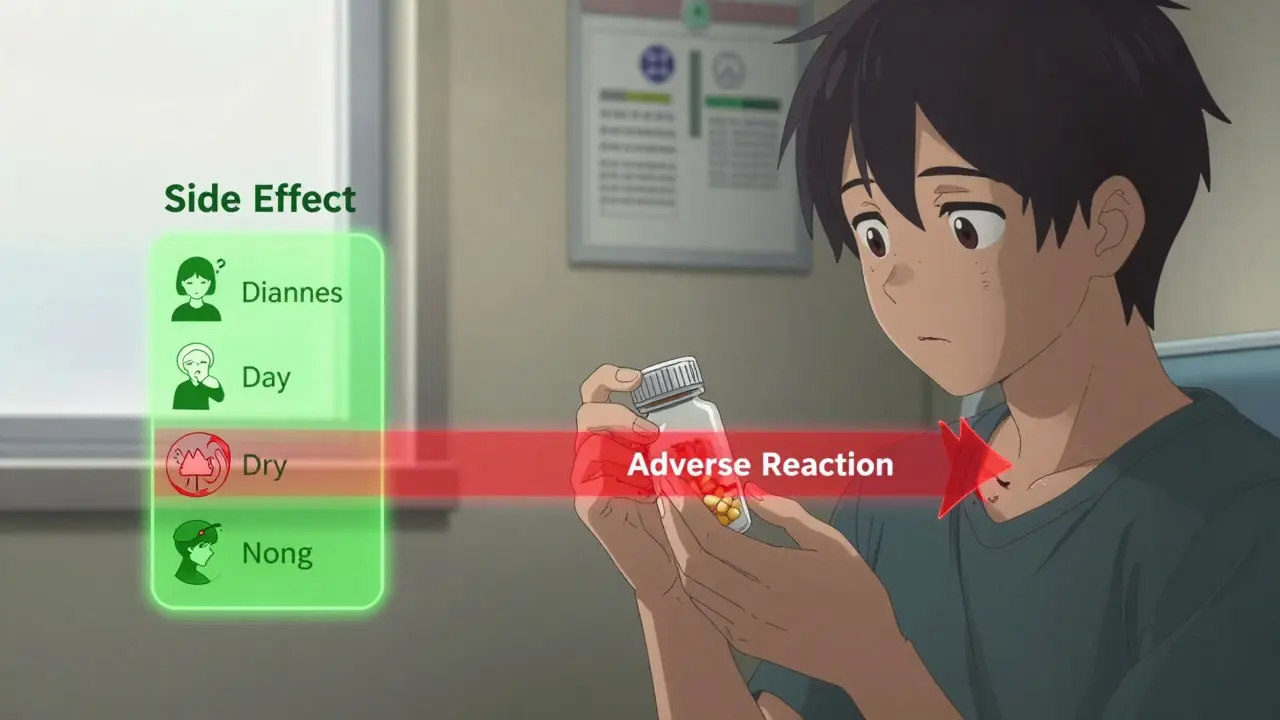
Here’s a simple way to think about it:- Side effect = Known, predictable, dose-related, happens often enough to be proven in trials.
- Adverse drug reaction = Includes side effects + rare, unexpected, serious reactions.
- Adverse event = Any bad thing that happens after you take a drug - whether it’s the drug’s fault or not.
- Check the drug’s official side effect list. Is it there? If yes, it’s likely a side effect.
- If it’s not on the list, is it something serious? Dizziness? Maybe. Chest pain? Call your doctor.
- Did it start right after you took the drug? Or did it happen weeks later? Timing matters.
- Have you had this before? Maybe it’s unrelated - like a virus or stress.
What’s Changing in the Field
Technology is helping. New AI tools can now scan millions of patient reports and flag patterns that humans miss. In 2023, one study showed AI improved side effect identification accuracy by 41%. The WHO updated its drug dictionary in March 2024 to include over 14,000 confirmed side effects - up from 11,600 in 2021. That’s more clarity. And genetic testing is starting to play a role. Some people have genes that make them more likely to have certain side effects. For example, people with a specific CYP2C19 gene variant are nearly nine times more likely to bleed from the blood thinner clopidogrel. That’s not random. That’s personalized risk. The FDA is now requiring AI systems used in drug safety to prove they can tell the difference between adverse events and side effects. By 2025, that’ll be mandatory.What You Should Do
You don’t need to memorize medical jargon. But you do need to be smart about how you talk about your meds.- Don’t say "side effect" unless you’re sure it’s listed in the official info.
- Use "I had this symptom after starting the drug" instead of "this is a side effect."
- Report anything unusual to your doctor - even if you think it’s "just a side effect."
- Ask your pharmacist: "Is this a known side effect, or could it be something else?"
Are side effects the same as adverse drug reactions?
No. All side effects are a type of adverse drug reaction, but not all adverse drug reactions are side effects. Side effects are predictable, dose-related reactions that happen because of how the drug works. Adverse drug reactions include those - plus rare, unexpected, and sometimes serious reactions that aren’t tied to the drug’s main action, like allergic responses or sudden organ damage.
Can an adverse event be a side effect?
An adverse event is any negative health occurrence after taking a drug - whether it’s caused by the drug or not. It only becomes a side effect after researchers prove through clinical trials that the drug caused it. For example, if a patient gets a headache after starting a new pill, that’s an adverse event. If many patients on the drug get headaches - and people on placebo don’t - then it’s confirmed as a side effect.
Why do drug labels say "side effects" if the medical term is "adverse reaction"?
Drug labels use "side effects" because it’s simpler for patients to understand. The FDA allows this in patient-facing materials, even though professionals use "adverse reaction" for confirmed cases. In scientific documents, the terms are kept separate. But in everyday use, "side effect" has become the common term - even if it’s not technically precise.
What should I do if I think I’m having an adverse reaction?
If you experience a serious symptom - like chest pain, trouble breathing, swelling, rash, or unusual bleeding - contact your doctor or go to urgent care immediately. Don’t wait. For less serious symptoms, write them down: when they started, how bad they are, and if anything made them better or worse. Then talk to your pharmacist or doctor. They can check if it’s a known side effect or something that needs more investigation.
Can I stop my medication if I think I’m having side effects?
Never stop a prescribed medication without talking to your doctor first. Many symptoms people blame on drugs are actually caused by other things - stress, illness, or even aging. Stopping a drug like blood pressure medicine, antidepressants, or anticoagulants suddenly can be dangerous. Always report the symptom, get it checked, and let your doctor decide if the drug needs to change.




Comments (8)