Ankylosing Spondylitis: Causes, Symptoms, and Treatment Options
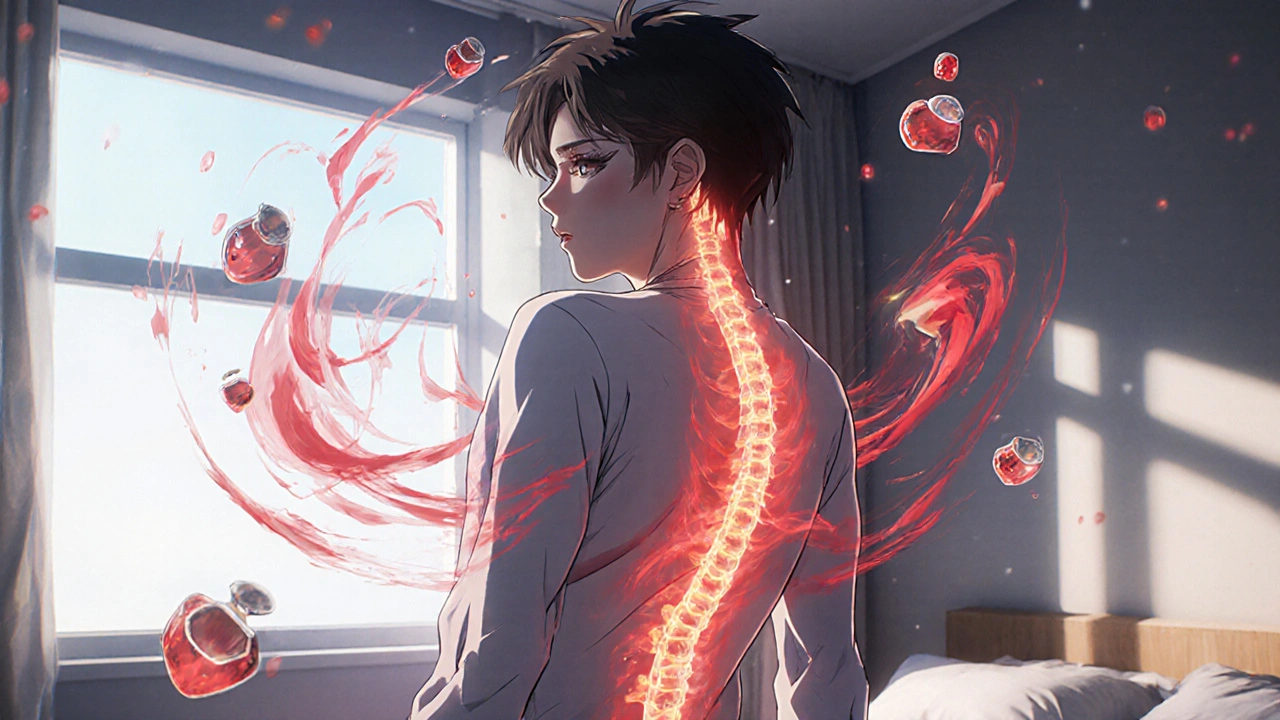
When your spine starts to fuse together because of chronic inflammation, you’re dealing with ankylosing spondylitis, a type of arthritis that primarily targets the spine and sacroiliac joints, leading to pain, stiffness, and over time, bone fusion. Also known as Axial Spondyloarthritis, it’s not just back pain—it’s an autoimmune disease where your immune system attacks your own joints, especially in young adults.
This condition doesn’t just affect your spine. It can also cause inflammation in the eyes, heart valves, and even the lungs. Many people first notice symptoms in their late teens or early 20s—morning stiffness that lasts over 30 minutes, pain that improves with movement but gets worse with rest, and a gradual loss of flexibility. It’s often mistaken for a simple strain, but if it’s been going on for more than three months, it’s worth getting checked. The HLA-B27 gene is strongly linked to it, though not everyone with the gene develops the disease. And while it’s more common in men, women get it too, often with milder symptoms that get missed.
There’s no cure, but early treatment can stop or slow down the damage. The first line of defense is usually NSAIDs, like naproxen or celecoxib, which reduce inflammation and ease pain for most people. If those don’t cut it, doctors turn to biologic treatments—drugs like adalimumab or etanercept—that block specific parts of the immune system causing the inflammation. These aren’t cheap, but they can change the game. Physical therapy is just as important as medication. Stretching, swimming, and posture training help keep your spine mobile and prevent permanent bending.
What you eat, how you sleep, and whether you smoke all matter. Smoking makes ankylosing spondylitis worse—faster fusion, more pain, less response to treatment. Cutting out cigarettes is one of the most effective things you can do. And while supplements like omega-3s or turmeric might help a little, they don’t replace proven treatments. You’ll also want to monitor for complications: uveitis (eye inflammation), osteoporosis, and heart issues can sneak up if you’re not careful.
The posts below cover real-world strategies you won’t find in brochures. You’ll see how hydroxychloroquine is sometimes used off-label, how NSAIDs interact with other meds, what lab markers doctors track to monitor flare-ups, and how patient feedback helps shape treatment guidelines. Some posts dive into the science behind biologics, others give practical tips for managing stiffness at work or during travel. This isn’t theoretical—it’s what people are actually doing to live better with this condition.