C3 Glomerulonephritis: Causes, Diagnosis, and Treatment Options
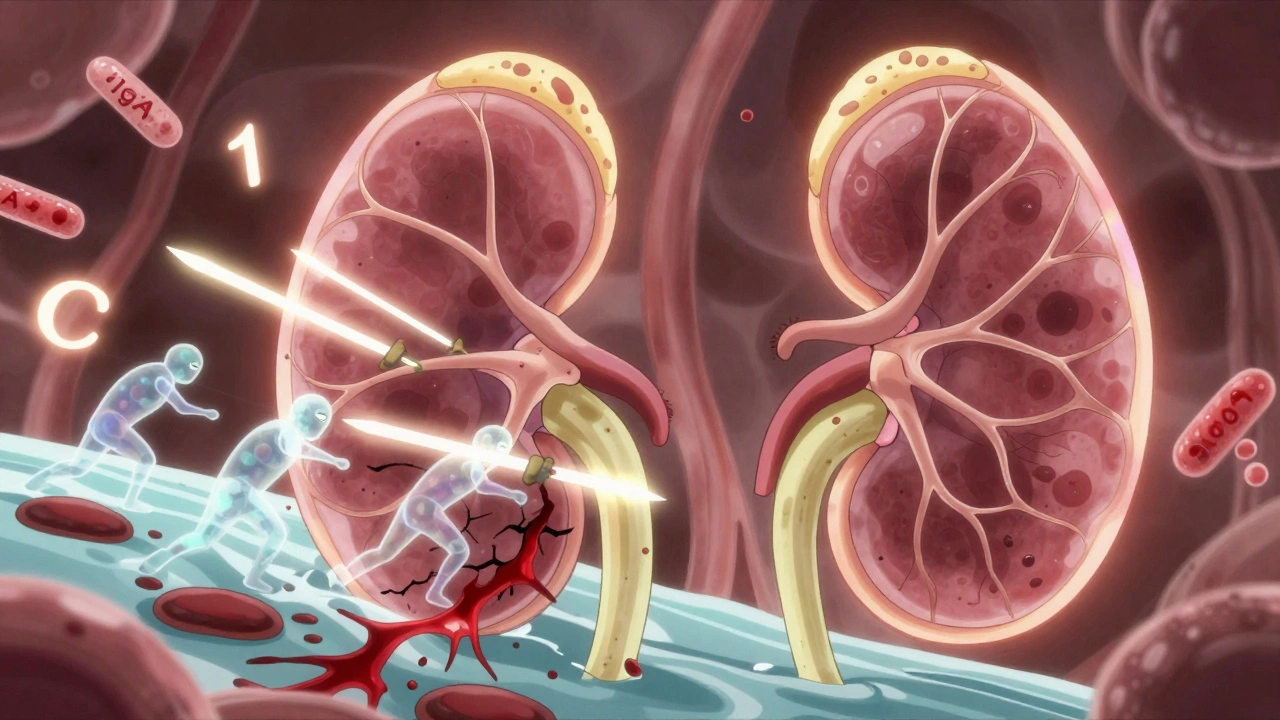
When your C3 glomerulonephritis, a rare kidney disease caused by uncontrolled activation of the complement system that damages the filtering units of the kidneys. Also known as C3 GN, it’s not caused by infections or diabetes—it’s an autoimmune glitch where your body’s own defense system attacks your kidneys. Unlike other kidney diseases, C3 glomerulonephritis doesn’t show up with high levels of antibodies. Instead, it’s marked by abnormal buildup of a protein called C3 in the kidney filters, leading to blood and protein leaking into urine. This is why a renal biopsy, the only definitive way to diagnose C3 glomerulonephritis by examining kidney tissue under a microscope is non-negotiable. Without it, you might mistake it for lupus nephritis or IgA nephropathy—and get the wrong treatment.
The complement system, a group of proteins that normally fight infections but can turn destructive when misregulated is at the heart of this disease. In C3 glomerulonephritis, something goes wrong—either a genetic mutation, an autoantibody, or a combination—that keeps the C3 protein spinning out of control. This isn’t a slow creep; it can crash kidney function in months. Some patients develop high blood pressure, swelling in the legs, or foamy urine long before they feel sick. Others show up with acute kidney failure. There’s no single trigger, but family history, recent infections, or other autoimmune conditions can raise your risk.
Treatment isn’t one-size-fits-all. Some patients respond to immunosuppressants, medications like corticosteroids or cyclophosphamide that dampen the overactive immune response. Others need drugs targeting the complement system directly—like eculizumab or ravulizumab—which block the specific proteins causing the damage. But these are expensive, not always covered, and not guaranteed to work. Many doctors start with the safest, cheapest options first and only escalate if the disease keeps progressing. What matters most is catching it early. Once scarring sets in, kidney damage is permanent.
You won’t find C3 glomerulonephritis in mainstream health articles. It’s rare, complex, and often misunderstood—even by some specialists. That’s why the posts here focus on real-world challenges: how to interpret biopsy results, when to push for a second opinion, how to manage side effects from long-term steroid use, and what lifestyle changes actually help preserve kidney function. You’ll also find practical advice on navigating insurance for rare disease drugs, tracking lab values between appointments, and recognizing warning signs before another flare hits. This isn’t theory. It’s what patients and nephrologists are dealing with right now.