Generic Drug Delay: Why Cheap Medicines Take Longer to Reach You
When you hear generic drug delay, the period between a brand-name drug’s patent expiration and when affordable copies become available. Also known as generic market entry delay, it’s not just a paperwork issue—it’s a barrier that keeps millions paying hundreds more for the same medicine. This delay isn’t accidental. It’s built into the system by legal loopholes, patent extensions, and corporate strategies that stretch exclusivity far beyond what Congress originally intended.
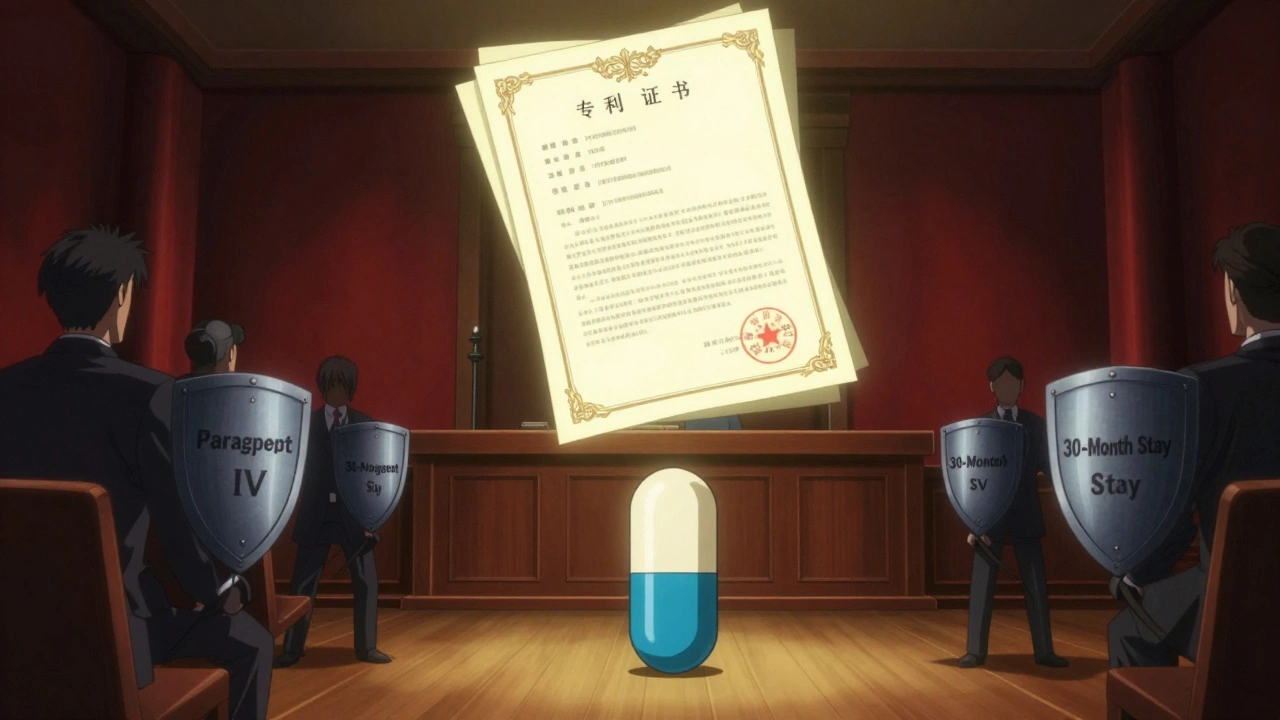
One major cause is formulation patents, patents on how a drug is made—its pill shape, coating, or combination with other ingredients. Even after the original chemical patent expires, companies file new ones on these minor changes. This resets the clock, blocking generics for years. Another is biosimilars, lower-cost versions of complex biologic drugs like Humira or Enbrel. Unlike regular generics, biosimilars face 12 years of exclusivity and complex legal battles before they can enter the U.S. market, even when the science says they’re safe. Then there’s patent thickets, a web of dozens of overlapping patents that make it risky and expensive for generic makers to challenge. Many simply give up. The result? A drug that should cost $5 a month still sells for $150 because no competitor can legally enter.
These delays aren’t theoretical. They hit people with diabetes, arthritis, and high blood pressure hardest. A 2023 study found that 40% of patients skipped doses or cut pills in half because they couldn’t afford the brand-name version—even after the patent expired. Meanwhile, the companies that own those patents kept billions in profits. The system rewards legal maneuvering over patient access.
What’s worse, these delays often go unnoticed. You might think your pharmacy ran out of stock. Or that the drug is "in short supply." But the real reason? No generic has been cleared to sell yet. And when one finally does, the price doesn’t always drop fast. Middlemen, pharmacy benefit managers, and distributors often keep the savings, not the patient.
But change is coming. More regulators are cracking down on evergreening tactics. Some states now require transparency on why a generic hasn’t launched. And patients are starting to ask: "Why is this still expensive?" The posts below show real cases—how a simple change in pill coating delayed a diabetes drug for seven years, how a biologic’s patent thicket blocked 14 biosimilar attempts, and how one company fought a generic for 11 years using nothing but paperwork.
You’ll find stories of people who paid too much, pharmacists who saw the pattern, and the legal tools now being used to break these delays. This isn’t about theory. It’s about the pills in your bottle—and why they cost what they do.