Nocebo Effect: How Negative Expectations Can Make You Feel Worse
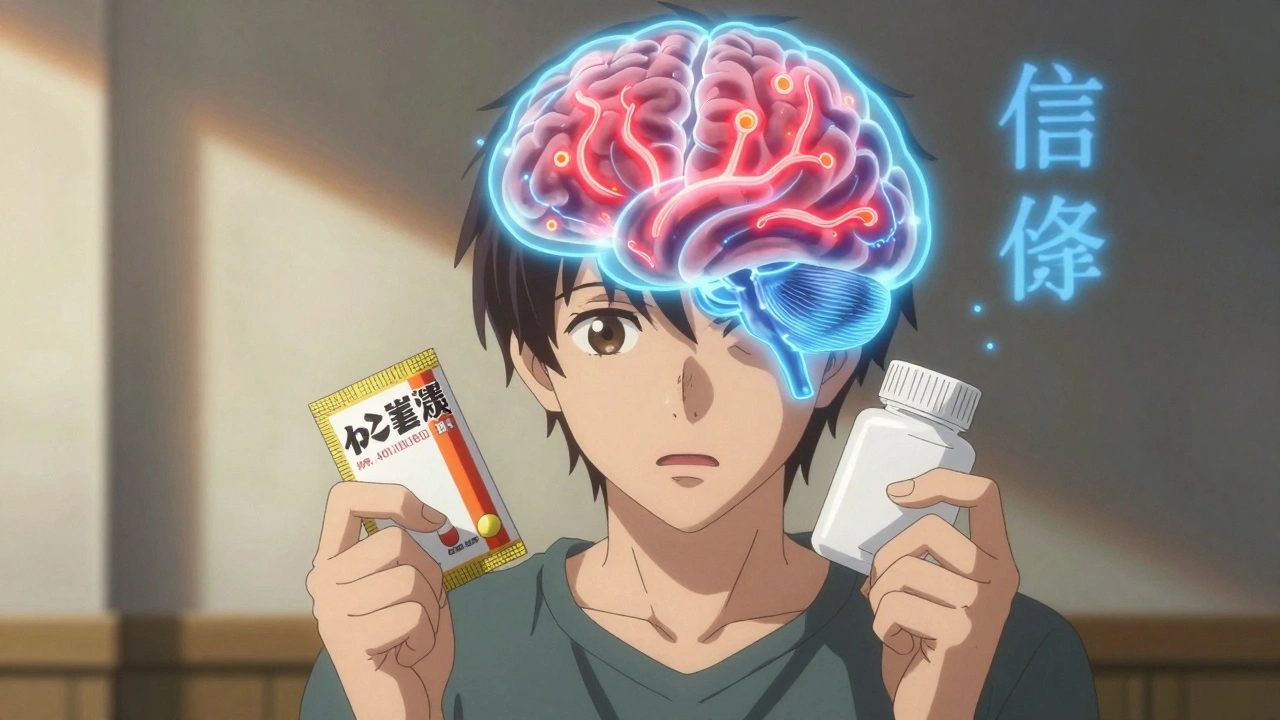
When you expect a medication to make you feel sick, it often does—nocebo effect, the harmful counterpart to the placebo effect, where negative beliefs trigger real physical symptoms. It’s not in your head—it’s in your body. Your brain hears "this drug causes dizziness" and your nervous system delivers it, even if the pill is sugar. This isn’t rare. Studies show up to 75% of people in placebo groups report side effects like headaches, nausea, or fatigue simply because they were told those symptoms were possible.
The placebo effect, the positive response to an inert treatment due to belief in its benefit gets all the attention, but the nocebo effect, the harmful counterpart to the placebo effect, where negative beliefs trigger real physical symptoms is just as powerful—and often ignored by doctors. If a patient reads a long list of side effects on a prescription label, they’re more likely to experience them. That’s not weakness. That’s biology. Your brain doesn’t distinguish between a real threat and a warned-about one. The same neural pathways light up whether you’re poisoned or just told you might be. This matters because patient expectations, the beliefs and assumptions patients hold about a treatment’s outcomes, which directly influence their physical and emotional responses shape everything from pain levels to recovery speed. A patient who believes their medication will cause drowsiness may drive poorly—not because the drug is strong, but because their mind made it so.
Doctors aren’t always trained to handle this. They focus on what the drug does, not what the patient thinks it does. But when a patient says, "I got dizzy after taking this," and the doctor says, "That’s normal," it reinforces the fear. Worse, if the patient Googles the drug and finds horror stories, the nocebo effect multiplies. This isn’t just about pills—it shows up in vaccines, surgeries, even supplements. The drug side effects, unwanted physical or mental reactions caused by medications, which can be amplified by psychological factors like fear or misinformation you read about aren’t always the drug’s fault. Sometimes, they’re your mind’s echo.
There’s a way out. Clear, calm communication from providers can cut nocebo responses by half. Instead of listing every possible side effect, say: "Most people feel fine. A few get mild nausea, which usually fades in a few days." That’s not hiding information—it’s reducing harm. And when you’re the patient, knowing this exists helps. If you start feeling weird after a new med, pause. Is it the drug? Or did you just read too many reviews? Your body listens to your mind. Sometimes, the best medicine is a quieter expectation.
Below, you’ll find real stories and science-backed insights from patients and providers who’ve seen this play out—from how antihistamines cause drowsiness not just chemically but psychologically, to why some people feel worse on generics simply because they believe they’re "lesser." These aren’t myths. They’re measurable, repeatable, and preventable. Let’s look at how it really works.