Patent Expiration: What Happens When Drug Monopolies End
When a drug’s patent expiration, the legal end of a drug company’s exclusive right to sell a medication. Also known as drug patent cliff, it’s when generic versions can legally enter the market and prices usually drop—sometimes by over 95%. But the moment the patent expires doesn’t always mean instant savings. Many drugs stay expensive for years because companies use tricks to stretch their control.
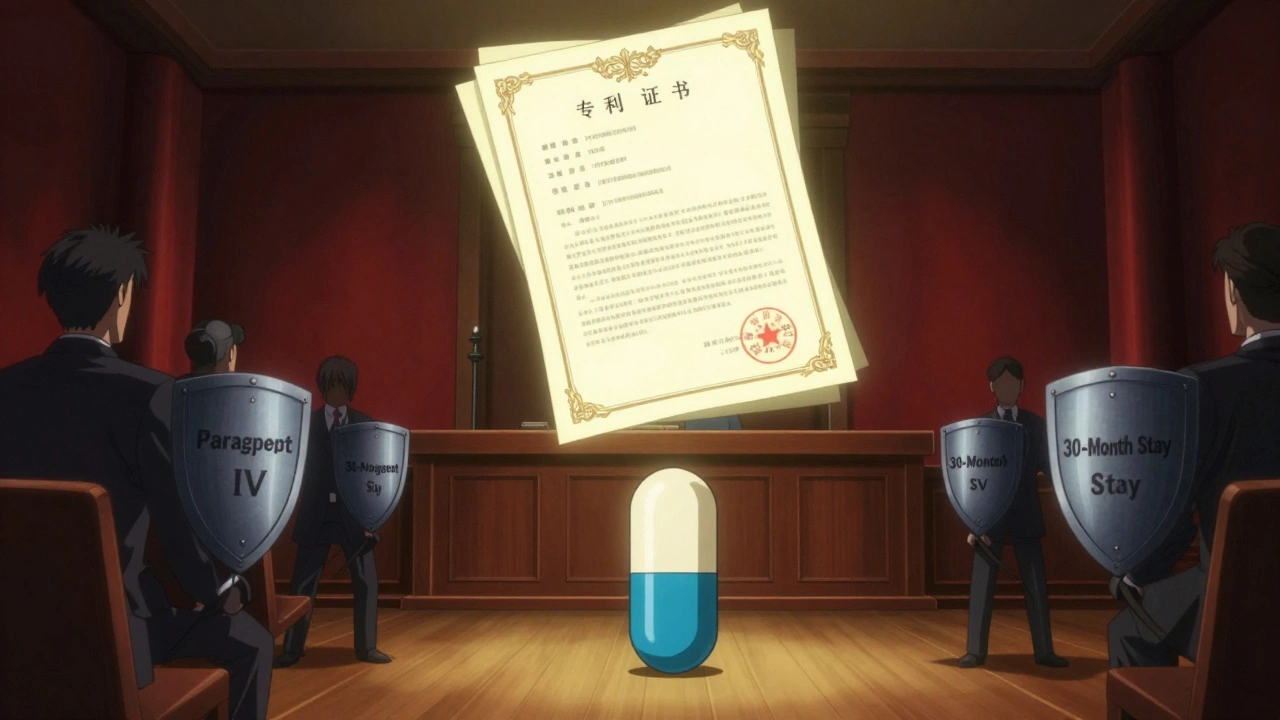
One big trick is formulation patents, patents on how a drug is made—like its pill shape, timing, or combo with other ingredients. These let companies claim a new invention even when the original active ingredient is old. Another is biologic patent protection, special rules that give biologic drugs 12 years of market exclusivity before biosimilars can even apply to be sold. Unlike regular generics, biosimilars aren’t exact copies, so they face higher hurdles and costs to get approved. And then there’s evergreening, the practice of filing new patents on minor changes just before the old one runs out. It’s not illegal, but it keeps prices high and delays real competition.
These tactics aren’t just corporate strategy—they hit your pocketbook. A drug that should’ve become cheap after patent expiration might still cost hundreds because no generic is available yet. You might see ads for the brand-name version long after it should’ve lost its monopoly. Meanwhile, people who need daily meds—like insulin, asthma inhalers, or blood pressure pills—end up paying more than they should. The system was meant to reward innovation, but too often it rewards delay.
That’s why the posts below dig into the real-world impact. You’ll find how generic drug price wars actually work, why some people still distrust generics even when they’re proven safe, and how biosimilars are slowly breaking into the market after years of legal battles. You’ll see how companies use patent loopholes to keep drugs expensive, and how you can spot when a drug is finally due for a price drop. Some posts even show how patient feedback and regulatory rules are starting to push back against these delays. This isn’t just about law or business—it’s about whether you can afford to stay healthy.