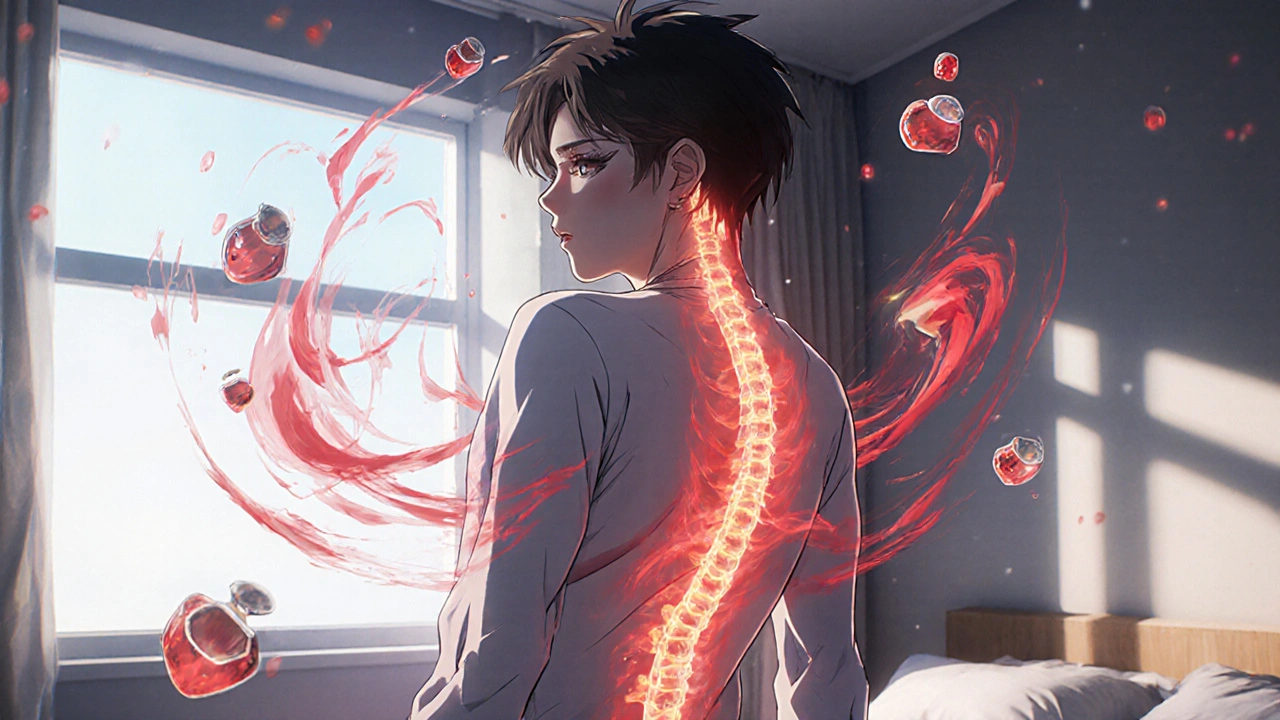
Spine Inflammation: Causes, Symptoms, and How It Connects to Autoimmune Diseases
When your spine inflammation, a condition where the vertebrae or surrounding tissues become swollen and irritated. Also known as spondylitis, it doesn't just hurt—it can limit how you move, sleep, and even breathe over time. This isn't just old age or a bad posture. It’s often a sign your immune system is attacking your own joints, especially in conditions like rheumatoid arthritis, an autoimmune disorder that targets joint linings, including those in the spine. Many people don’t realize spine inflammation can be the first warning sign of something deeper, not just a sore back from sitting too long.
It’s not just about pain. Spine inflammation often comes with morning stiffness that lasts more than 30 minutes, fatigue that won’t quit, and sometimes even eye redness or digestive issues. These aren’t random symptoms—they’re clues. The same immune overactivity that causes autoimmune disease, a group of conditions where the body attacks healthy tissue in the joints can also trigger inflammation in the spine. That’s why people with rheumatoid arthritis, ankylosing spondylitis, or lupus often report spinal symptoms early on. And if you’re being treated for one of these conditions, your spine pain isn’t just a side effect—it’s part of the disease itself.
What’s surprising is how often spine inflammation gets missed. Doctors might blame it on muscle strain, order an X-ray that shows nothing, and send you home with painkillers. But early-stage inflammation doesn’t always show up on regular scans. It needs an MRI or a blood test for markers like CRP or ESR to confirm. And treatment? It’s not just about popping NSAIDs. Managing it often means working with your care team to control the root cause—your immune system. That’s where drugs like methotrexate or biologics come in, the same ones used for autoimmune disease monitoring, tracking flares and damage through lab tests and imaging. Skipping this step means you’re treating the symptom, not the problem.
You’ll find posts here that dig into how spine inflammation connects to other conditions—like how hydroxychloroquine is still used in some autoimmune cases, or how NSAIDs like aceclofenac help with pain but come with risks when mixed with antidepressants. There’s also real talk about what works: when physical therapy helps, when surgery is needed, and why some people find relief through diet and sleep, not just pills. This isn’t a list of quick fixes. It’s a collection of practical, evidence-backed insights from people who’ve lived with this—and the experts who treat it.