If you're pregnant or planning to be, and you're on warfarin, you're probably worried. You're not alone. Thousands of women every year face this exact dilemma: they need to manage a serious medical condition like atrial fibrillation, a mechanical heart valve, or a history of blood clots - but now they're carrying a baby. And warfarin, the drug that’s kept them safe for years, might be putting that baby at risk.
Why Warfarin Is Dangerous During Pregnancy
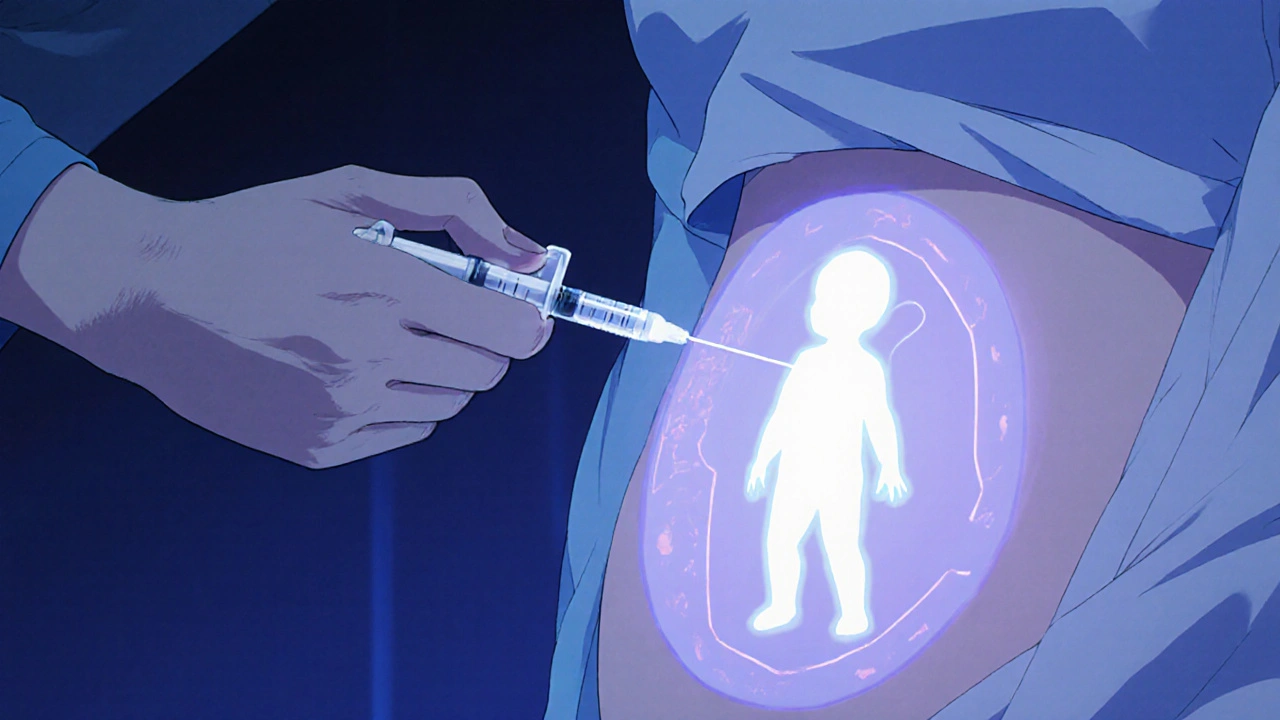
Warfarin crosses the placenta. That means it doesn’t just stay in your bloodstream - it reaches your developing baby. And that’s where the danger starts.
Between weeks 6 and 12 of pregnancy, warfarin can cause fetal warfarin syndrome. This isn’t rare. Studies show up to 1 in 5 babies exposed to warfarin during this window develop serious birth defects. These include underdeveloped noses, bone abnormalities, eye problems, and developmental delays. The risk drops after week 12, but even later in pregnancy, warfarin can cause bleeding inside the baby’s brain - a life-threatening complication.
The U.S. Food and Drug Administration classifies warfarin as a Category X drug for pregnancy. That’s the highest risk category - meaning the dangers clearly outweigh any possible benefits. It’s not a suggestion. It’s a warning built on decades of clinical data.
What Alternatives Are Safe?
Good news: there are safer options. Low molecular weight heparin (LMWH), like enoxaparin (Lovenox) or dalteparin (Fragmin), is the gold standard for pregnant women who need anticoagulation.
Unlike warfarin, heparin doesn’t cross the placenta. It stays in your blood, protecting you from clots without touching your baby. It’s given as a daily injection under the skin - not a pill - but many women find the routine manageable. Studies tracking over 1,500 pregnancies show LMWH has a safety profile similar to no medication at all when used correctly.
Unfractionated heparin is another option, especially if you’re at high risk for clots or have kidney issues. It requires more frequent monitoring but works just as well. Both types are approved for use throughout all three trimesters.
When Can You Go Back to Warfarin?
After delivery, warfarin becomes safe again. In fact, it’s often the best choice for postpartum care, especially if you have a mechanical heart valve or a history of recurrent clots.
You can start taking warfarin as soon as 24 to 48 hours after birth - even if you’re breastfeeding. Warfarin passes into breast milk in tiny, harmless amounts. The American College of Obstetricians and Gynecologists confirms it’s safe for nursing mothers.
But here’s the catch: you can’t just switch back on your own. Your doctor will need to monitor your INR levels closely. Warfarin’s effect changes after pregnancy - your body’s metabolism shifts, and your dose might need adjusting. Don’t assume your pre-pregnancy dose is still right.
Planning Ahead: What to Do Before You Get Pregnant
If you’re thinking about getting pregnant and you’re on warfarin, don’t wait. Talk to your doctor now.
Here’s what you need to do:
- Get your INR levels stable - ideally between 2.0 and 3.0 - before conception.
- Switch to heparin at least one month before trying to conceive. This gives your body time to adjust.
- Find a high-risk pregnancy specialist (maternal-fetal medicine doctor) who’s experienced with anticoagulation.
- Make sure your cardiologist and OB-GYN are communicating. Coordination saves lives.
- Keep a written log of your injections, dates, and any side effects. Bring it to every appointment.
Many women think, “I’ll just stop warfarin and hope I don’t clot.” That’s dangerous. Stopping blood thinners suddenly can trigger a clot in your lungs, heart, or brain - which could kill you and your baby. Never stop or change your meds without medical supervision.
What If You Got Pregnant While on Warfarin?
It happens. More often than you’d think. Maybe you didn’t know you were pregnant. Maybe you missed a period. Maybe you thought you were safe because you weren’t using birth control.
If you find out you’re pregnant while taking warfarin, don’t panic. Don’t blame yourself. Do this:
- Call your doctor immediately - even if you feel fine.
- Stop warfarin right away - but don’t stop cold. Your doctor will likely start you on heparin within 24 hours.
- Get an early ultrasound, ideally between weeks 10 and 12. This checks for signs of fetal warfarin syndrome.
- Consider a detailed anatomy scan at week 20. It can catch structural problems early.
Many women who accidentally take warfarin early in pregnancy go on to have healthy babies - especially if they switch to heparin quickly. Timing matters. The sooner you switch, the better the outcome.
Monitoring Your Health During Pregnancy
Switching to heparin doesn’t mean you’re out of the woods. You still need close monitoring.
Here’s what your care plan should include:
- Weekly blood tests for the first trimester, then every 2-4 weeks after.
- Regular ultrasounds to check fetal growth and movement.
- Consultations with a hematologist to adjust your heparin dose as your pregnancy progresses.
- Monitoring for signs of heparin-induced thrombocytopenia (HIT), a rare but serious drop in platelets.
Some women need higher doses of heparin as their blood volume increases. Others need less. There’s no one-size-fits-all. Your dose is based on your weight, your condition, and your lab results - not a chart or guesswork.
Delivery and Postpartum Planning
How you deliver matters. If you’re on heparin, your doctor will likely stop it 24 hours before labor starts to reduce bleeding risk. If you’re having a C-section, they might stop it even earlier.
After delivery, you’ll likely be switched back to warfarin - but not always. Some women stay on heparin for a few weeks, especially if they had a C-section or complications. Others go straight to warfarin. Your doctor will decide based on your clotting risk and recovery.
Don’t forget: you’re still at high risk for clots in the first 6 to 12 weeks after birth. That’s when most pregnancy-related blood clots happen. Keep your follow-up appointments. Don’t ignore leg swelling, chest pain, or sudden shortness of breath.
Emotional Support Matters Too
Managing a chronic condition during pregnancy is stressful. You’re not just worried about your baby - you’re worried about your future, your independence, your identity as a healthy person.
Many women feel guilty about needing injections. Others feel isolated because no one else they know is going through this. That’s normal.
Find support. Join a group for women on anticoagulants during pregnancy. Talk to your partner. Don’t bottle it up. Mental health is part of your physical health - especially when you’re managing a high-risk pregnancy.
Bottom Line: You Can Have a Healthy Pregnancy on Blood Thinners
Warfarin and pregnancy don’t mix. But you don’t have to give up your health to have a baby. With the right plan - and the right team - you can manage your condition and carry a healthy child.
Switch from warfarin to heparin before conception. Stick to your monitoring schedule. Communicate with your doctors. And remember: you’re not alone. Thousands of women have walked this path before you - and come out on the other side with a healthy baby and their own health intact.
Can I take warfarin while breastfeeding?
Yes. Warfarin passes into breast milk in very small amounts that are not harmful to the baby. The American College of Obstetricians and Gynecologists confirms it’s safe for nursing mothers. Most women switch back to warfarin after delivery because it’s easier to take than daily injections and works well for long-term management.
Is there a pill form of heparin?
No. Heparin, including low molecular weight heparin (LMWH), must be injected under the skin. There are no oral anticoagulants approved for use during pregnancy besides warfarin - and warfarin is dangerous in pregnancy. That’s why injections are necessary. While it’s inconvenient, most women adapt quickly and find the routine manageable with practice.
What are the signs of fetal warfarin syndrome?
Signs include a flattened or underdeveloped nose, small head size, bone abnormalities (especially in the spine and limbs), eye problems like cataracts or small eyes, and developmental delays. These typically appear when warfarin is taken between weeks 6 and 12 of pregnancy. An early ultrasound at 10-12 weeks can detect many of these issues.
Can I use DOACs like apixaban or rivaroxaban during pregnancy?
No. Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran are not approved for use during pregnancy. They cross the placenta and may cause serious harm to the fetus. There’s not enough safety data to recommend them. Heparin remains the only safe, proven option.
How often do I need blood tests while on heparin during pregnancy?
You’ll typically need blood tests weekly during the first trimester, then every 2 to 4 weeks after that. Your doctor may adjust the frequency based on your weight gain, kidney function, and how your body responds to the dose. Unlike warfarin, you don’t need INR tests with heparin - instead, your doctor may check anti-Xa levels to make sure the dose is right.




Comments (14)