Every year, over 50,000 women in the UK are diagnosed with breast cancer. That’s more than 130 people every day. Many of these cases are caught early-not because someone felt a lump, but because of a routine mammogram. Screening isn’t about fear. It’s about catching cancer before it spreads, when treatment is simpler, less invasive, and more effective. But with so many guidelines out there, it’s easy to get confused: When should you start? How often should you go? Is 3D mammography worth it? And what happens after a diagnosis?
When Should You Start Screening?
The answer used to be: start at 50. But that changed. In 2024, the American College of Obstetricians and Gynecologists (ACOG) updated its guidelines to say: start at 40. And they’re not alone. The U.S. Preventive Services Task Force (USPSTF), the American Cancer Society, and the National Comprehensive Cancer Network now all agree that women at average risk should begin screening mammography by age 40.
Why the shift? Data. Studies show breast cancer is rising in women under 50. More invasive cases are being found in their 40s. A 2016 meta-analysis of nine clinical trials found screening reduces breast cancer deaths by about 12% in women aged 39 to 74. That number might seem small, but when you’re talking about thousands of lives, it matters. Waiting until 50 means missing years where cancer can grow unnoticed.
For women aged 40 to 44, screening is optional-but strongly encouraged. From 45 to 54, annual mammograms are recommended. After 55, you can switch to every two years if you prefer, or keep going yearly. The key is this: don’t stop just because you hit a certain age. As long as you’re in good health and have a life expectancy of at least 10 years, screening continues to make sense.
2D vs. 3D Mammography: What’s the Difference?
Most women still get 2D mammograms. It’s simple: two X-ray images of each breast, from top and side. But 3D mammography-also called digital breast tomosynthesis (DBT)-is changing the game.
Instead of two flat pictures, DBT takes dozens of low-dose X-rays from different angles, then builds a 3D model of your breast tissue. Think of it like flipping through layers of a cake instead of seeing just the top and side. This helps doctors see through overlapping tissue, which is especially helpful if you have dense breasts.
Dense breasts mean more glandular and fibrous tissue, which shows up white on a mammogram-just like tumors. That’s why up to half of cancers in dense breasts are missed on 2D scans. DBT cuts those false negatives by up to 40%. It also reduces the chance of being called back for extra tests because of unclear results.
Most guidelines say both 2D and 3D are effective. But the American Society of Breast Surgeons says 3D should be the preferred method. Medicare covers both, and many insurers now cover DBT without extra cost. If you have dense breasts, a family history, or just want the clearest possible scan, ask for 3D. It’s not a luxury-it’s better detection.
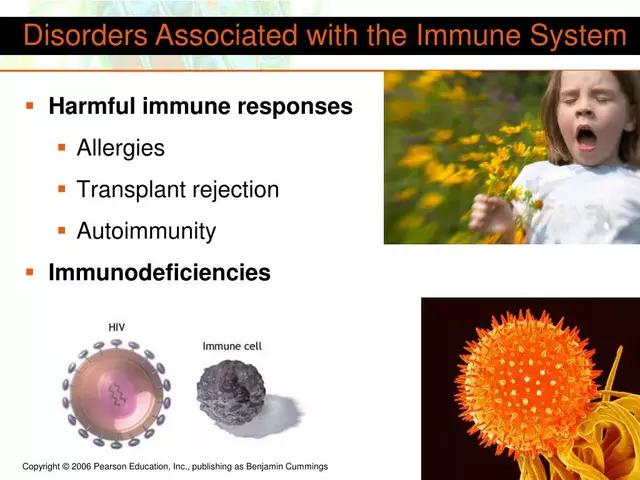
Who Needs Extra Screening?
Not everyone is average risk. If you’ve had radiation to the chest before age 30, carry a BRCA1 or BRCA2 mutation, or have a lifetime risk of breast cancer over 20%, your screening plan changes.
For these women, guidelines recommend two tools: yearly mammography and yearly breast MRI. MRI is far more sensitive than mammography alone. It can spot cancers that mammograms miss, especially in younger women or those with dense tissue. The American Cancer Society recommends starting MRI at age 30 for high-risk women.
What about dense breasts without other risk factors? Here’s where things get messy. The USPSTF says there’s not enough evidence to recommend routine ultrasound or MRI for dense breasts alone. But the American Cancer Society says women with heterogeneously or extremely dense breasts should consider supplemental screening. Many clinics now offer it as an option, even if insurance doesn’t cover it yet. If your mammogram says you have dense breasts, ask your doctor: Should I add an MRI or ultrasound?
And forget about breast self-exams. The Canadian Task Force and others have found no proof that checking your own breasts reduces deaths. Clinical breast exams by a provider? Also not proven to help. Stick to mammography-especially 3D-for reliable results.
What Happens After a Diagnosis?
Screening finds cancer. But treatment? That’s a whole different path. It starts with a biopsy. If cancer is confirmed, doctors look at three key things: tumor size (T), lymph node involvement (N), and whether it’s spread (M). That’s the TNM staging system.
Then come the biomarkers:
- Hormone receptor status: Is the cancer fueled by estrogen or progesterone? If yes, hormone therapy (like tamoxifen or aromatase inhibitors) will likely be part of treatment.
- HER2 status: Is the cancer overproducing the HER2 protein? If so, targeted drugs like trastuzumab (Herceptin) can be life-saving.
- Genomic tests: Tests like Oncotype DX or MammaPrint analyze how aggressive the cancer is. They help decide whether chemotherapy is truly needed-or if you can skip it.
Next, surgery. Two main options: breast-conserving surgery (lumpectomy) or mastectomy. Radiation usually follows lumpectomy. For mastectomy, radiation depends on tumor size and lymph node involvement.
Systemic treatments-chemotherapy, hormone therapy, targeted therapy-are chosen based on risk level, not just stage. A small, hormone-positive, low-grade tumor in a 68-year-old might need only hormone therapy. A larger, HER2-positive tumor in a 42-year-old? That’s likely chemo plus targeted drugs.
There’s no one-size-fits-all algorithm. But every treatment plan follows a simple rule: match the therapy to the biology of the tumor. That’s why genetic testing and pathology reports matter so much. Don’t rush into surgery without them.

What’s Changing in 2026?
Guidelines keep evolving. In 2024, ACOG’s shift to age-40 screening brought U.S. organizations into near-perfect alignment. That’s a big deal. Before, you’d get different advice depending on which doctor you saw. Now, most clinicians agree: start at 40, go yearly until 55, then switch to every two years if you choose.
3D mammography is becoming standard, not optional. Hospitals in the UK and U.S. are upgrading equipment. Medicare and many private insurers now cover it routinely. And for high-risk women, MRI is no longer a last resort-it’s part of the baseline plan.
One thing hasn’t changed: screening saves lives. The 12% reduction in breast cancer deaths isn’t theoretical. It’s real. It’s women who didn’t die because they had a scan before they felt anything.
What to Do Next
- If you’re 40 or older: Schedule your first mammogram if you haven’t already. Don’t wait for symptoms.
- If you’re under 40: Ask your doctor about family history. If you have a strong history (mother, sister, or aunt diagnosed before 50), ask about genetic testing.
- If you have dense breasts: Request a 3D mammogram. Ask if supplemental screening is right for you.
- If you’ve been diagnosed: Make sure you get full biomarker testing (ER, PR, HER2, genomic score) before deciding on treatment. Don’t accept a plan without it.
Screening isn’t perfect. False positives happen. Anxiety is real. But the alternative-waiting until you feel a lump-is riskier than any scan.
Do I still need mammograms after menopause?
Yes. Breast cancer risk increases with age, and most cases are diagnosed after 50. As long as you’re healthy and have a life expectancy of 10 years or more, continue screening. The benefit doesn’t disappear just because you’ve gone through menopause.
Is 3D mammography more expensive?
In the U.S., Medicare and most insurers cover 3D mammography at no extra cost when it’s used as the primary screening tool. In the UK, NHS currently offers 2D mammography as standard, but private clinics increasingly offer 3D. If you’re at high risk or have dense breasts, ask your doctor if you qualify for 3D through your provider.
Can I skip mammograms if I have no family history?
Yes, you still need them. About 85% of breast cancers occur in women with no family history. Genetics play a role, but most cases come from aging, hormones, and random cell changes. Screening isn’t just for high-risk people-it’s for everyone.
Should I get an MRI instead of a mammogram?
No-not as a replacement. MRI is more sensitive but also more likely to find false positives. It’s not meant to replace mammography. It’s meant to work alongside it, especially for high-risk women. Mammograms are still the best tool for population-wide screening.
What if I’m scared of radiation from mammograms?
The radiation dose from a mammogram is very low-about the same as you’d get from a cross-country flight. A 2D mammogram delivers less than 0.4 millisieverts. A 3D mammogram adds a little more, but still far below safety limits. The risk from radiation is far lower than the risk of missing a cancer.
Early detection doesn’t guarantee you’ll never get breast cancer. But it gives you the best shot at beating it. If you’re due for a mammogram, make the call. If you’re unsure, talk to your doctor. This isn’t about fear. It’s about taking control-before it’s too late.