Most people don’t think of HPV as a cancer cause. They think of it as something that causes warts - maybe something you catch during sex, maybe something you brush off. But here’s the truth: HPV is behind nearly 48,000 new cancer cases in the U.S. every year. And the fastest-growing ones aren’t the ones you’ve heard about for decades. They’re throat and anal cancers - cancers that are rising in men, especially those over 40.
What HPV-Related Cancers Actually Look Like
HPV doesn’t just cause cervical cancer. It causes six types of cancer in total. The big three you need to know are cervical, oropharyngeal (throat), and anal cancer. Of these, throat cancer is now the most common HPV-linked cancer in men. In fact, about 70% of all throat cancers in the U.S. are caused by HPV - mostly type 16. That’s more than cervical cancer in men, and it’s rising fast.
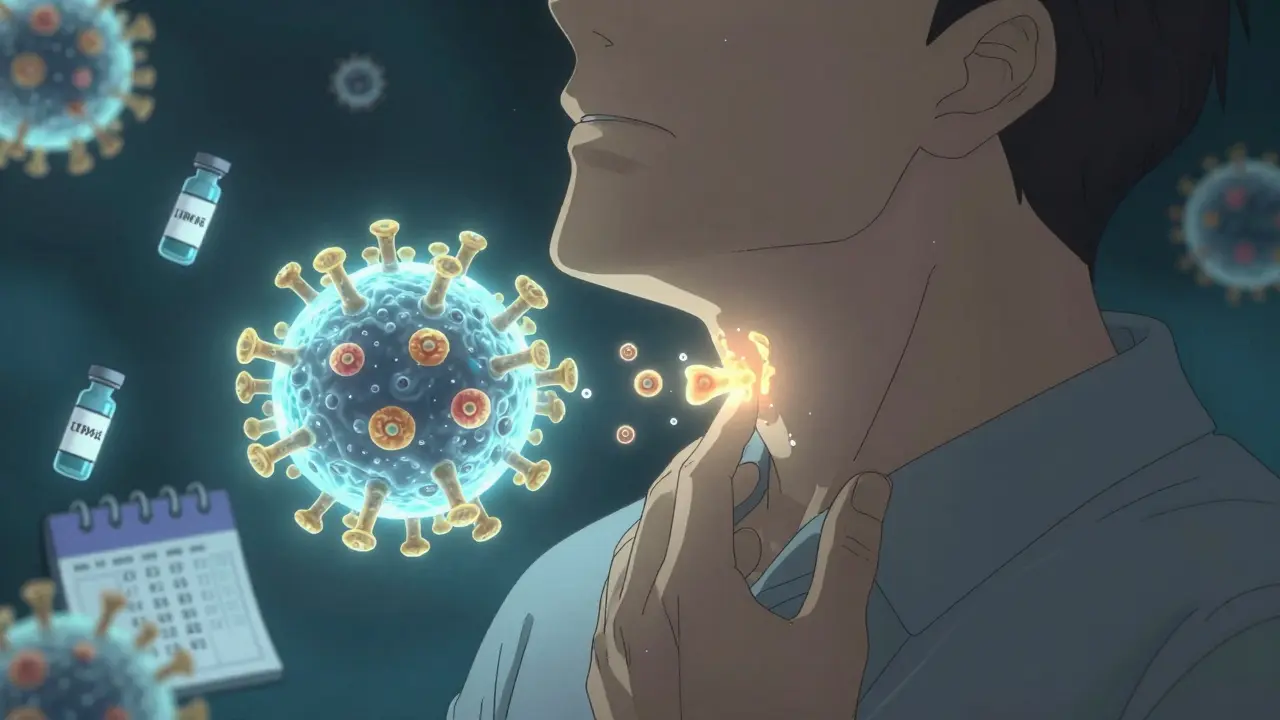
Throat cancer from HPV doesn’t always show up like smoking-related throat cancer. You won’t always have a hoarse voice or a persistent cough. Instead, you might notice a lump in your neck, trouble swallowing, or ear pain that won’t go away. It often shows up in people who’ve never smoked or drunk heavily. That’s why it catches so many off guard.
Anal cancer is less common but still serious. It’s linked to HPV in over 90% of cases. Symptoms include bleeding, itching, pain, or a lump near the anus. It’s often mistaken for hemorrhoids - and that delay in diagnosis can be dangerous. Both throat and anal cancers are more common in men than women, especially among White men aged 40 to 60.
Women still face the highest risk of cervical cancer, but screening has cut those numbers dramatically. Throat and anal cancers? No routine screening exists. That means prevention - not detection - is the only real defense.
Why HPV Is So Dangerous - And So Common
HPV isn’t rare. It’s one of the most common viruses on the planet. About 80% of sexually active people will get it at some point. Most infections go away on their own. But in about 1 in 10 people, the virus sticks around. That’s when it starts changing cells - slowly, silently - until they turn cancerous. It can take 10 to 30 years.
The real villains are HPV types 16 and 18. Together, they cause 70% of cervical cancers and 85% of HPV-positive throat cancers. Gardasil-9, the vaccine used today, protects against nine types, including 16 and 18. That’s why it prevents 90% of HPV-related cancers.
But here’s the problem: people think HPV is only a women’s issue. It’s not. Men get HPV. Men spread it. And men are now getting the majority of HPV-related cancers. Yet, vaccination rates for boys still lag behind girls. In 2022, only 65% of U.S. teens got all their HPV shots. That’s not enough.
How Vaccination Stops Cancer Before It Starts
The HPV vaccine is one of the most effective cancer-prevention tools ever made. It’s not just safe - it’s been studied in over 100 million people worldwide. Side effects? Mostly a sore arm or a brief fever. No link to long-term health problems.
The CDC recommends the vaccine for all kids at age 11 or 12. That’s because the immune system responds best before exposure. But it’s not too late for older teens and young adults. Anyone under 26 should get it. For adults 27 to 45, talk to your doctor - it may still help, especially if you haven’t been exposed to many HPV types.
Two doses are enough if you start before 15. After 15, you need three. The vaccine doesn’t treat existing infections - it prevents new ones. That’s why getting it early matters so much.
Real-world results are clear. In Australia, where vaccination started in 2007, cervical precancers dropped by 85% in young women. In the U.S., high-grade cervical lesions in teen girls fell by 80% since the vaccine arrived. And in countries like Denmark and Sweden, HPV-related throat cancers are already starting to decline in younger men.
One study in Rhode Island showed that putting vaccines in schools raised vaccination rates from 53% to 84% in just six years. That led to a 22% drop in dangerous cervical cell changes. This isn’t theory - it’s working.
Why Vaccination Rates Are Still Too Low
So why aren’t more kids getting the vaccine?
Parents worry about safety. But surveys show only 28% of parents refuse because they think it’s unsafe. The rest? They don’t think it’s necessary. Or they forget. Or their doctor doesn’t push it.
Doctors play a huge role. If a provider says, “Your child needs the HPV vaccine today,” vaccination rates jump. But only 65% of doctors consistently recommend it as strongly as other teen vaccines. Too many say, “You can get it next time,” or “Let’s wait.” That delay costs lives.
Access is another issue. In rural areas, 32% fewer clinics offer the vaccine. In some places, it’s not stocked. In others, it’s too expensive without insurance. Even with the Vaccines for Children program, many families don’t know it exists.
And then there’s stigma. People think HPV means promiscuity. That’s false. HPV is like the common cold - you can get it from one partner, even after years of monogamy. The virus doesn’t judge. But society does. And that silence keeps people from talking, from vaccinating, from getting screened.
Screening: What Works and What Doesn’t
For cervical cancer, we have a solid system: HPV testing every five years, or Pap smears every three. That’s why cervical cancer rates have dropped by half since the 1970s.
But for throat and anal cancer? No screening exists. No test can catch early changes in the throat. No routine anal Pap test is recommended for the general public. That’s why vaccination is the only reliable shield.
There are exceptions. Men who have sex with men and people with weakened immune systems (like those with HIV) are sometimes screened for anal cancer. But that’s not the norm. And even then, the tests aren’t perfect.
The best move? Don’t wait for symptoms. Don’t wait for screening. Get vaccinated. It’s the only proven way to stop these cancers before they start.

The Cost of Waiting
HPV-related cancers aren’t just deadly - they’re expensive. The average cost to treat throat cancer is nearly $200,000. Anal cancer? Around $135,000. Many patients lose their jobs. Some need feeding tubes. Others lose their voice permanently.
One man from Ohio, diagnosed with HPV-positive throat cancer at 48, told his story: “I couldn’t swallow for six months. I had a tube in my stomach. My voice is raspy now. My insurance covered most of it, but I still paid $127,000 out of pocket.”
That’s not an outlier. In 2022, HPV cancers cost the U.S. system $1.3 billion. And that doesn’t include lost wages, caregiving, or emotional toll.
Compare that to the vaccine: two or three shots, under $250 total. Often free with insurance. No recovery time. No scars. No feeding tubes.
What You Can Do Right Now
- If you’re a parent: Get your child vaccinated at 11 or 12. Don’t wait. It’s not about sex - it’s about cancer prevention.
- If you’re 13-26: If you haven’t been vaccinated, call your doctor. It’s not too late.
- If you’re 27-45: Talk to your provider. You might still benefit, especially if you’ve had few partners or never been vaccinated.
- If you’re a woman 25-65: Get screened for cervical cancer. HPV test every five years is best.
- If you’re a man: Don’t assume you’re safe. Talk to your doctor about HPV and your risk. Ask about the vaccine.
HPV doesn’t care about your gender, your income, or your relationship status. It only cares if your body is unprotected. The tools to stop it exist. The question is - will we use them?
Frequently Asked Questions
Can you get HPV from someone who doesn’t show symptoms?
Yes. Most people with HPV have no symptoms at all. They can still pass the virus to others through skin-to-skin contact during sex. That’s why vaccination is so important - it protects you even if you or your partner don’t know you’re infected.
Is the HPV vaccine only for girls?
No. The vaccine is for everyone. Boys and men can get HPV-related cancers too - especially throat and anal cancer. Vaccinating boys helps protect them and reduces spread to future partners. It’s not just a girls’ vaccine - it’s a cancer-prevention tool for all.
Can you get HPV even if you’ve only had one partner?
Absolutely. HPV is extremely common. You can get it from your first partner, even if they’ve never had another partner. It doesn’t mean anything about your behavior - it just means the virus is widespread and easy to catch.
Do I still need Pap tests if I got the HPV vaccine?
Yes. The vaccine doesn’t protect against all HPV types, and it doesn’t clear existing infections. Screening is still needed for women aged 25-65. The vaccine prevents cancer; screening catches early changes before they become cancer.
Is the HPV vaccine safe for adults over 26?
It’s not routinely recommended, but it may still help for people 27-45 who haven’t been exposed to many HPV types. Talk to your doctor. If you’ve had few partners or never been vaccinated, the benefits may outweigh the risks.
Can HPV cause cancer in people who never had sex?
It’s extremely rare. HPV spreads through intimate skin contact, usually during sexual activity. Non-sexual transmission (like through towels or surfaces) isn’t proven to cause cancer. The main route is sexual contact, so prevention focuses on vaccination and screening.




Comments (14)