Your bathroom medicine cabinet might be ruining your meds before you even take them. Every time you step into that steamy room, you're risking your health by keeping medication storage there. Here's why.
Why Your Bathroom Is a Meds Disaster Zone
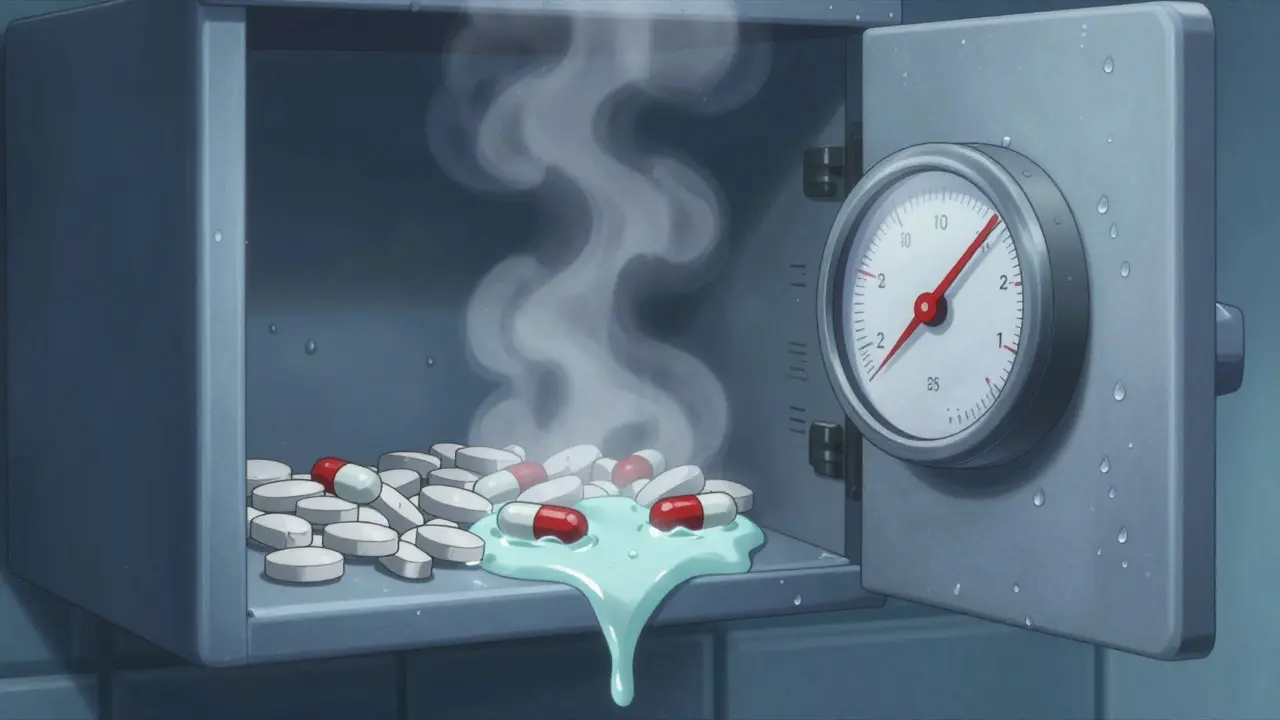
Think your bathroom medicine cabinet is safe? It's not. According to Thomas So, PharmD, senior manager of the Drug Information Group at First Databank, "prescription medications should never be stored in the bathroom for patient safety and safe drug use." Why? Bathrooms are humidity factories. Showers create steam that soaks everything. Relative humidity often hits 80-100% there-way above the safe 30-50% range for most meds. Plus, temperature swings wildly-from cool room temps to hot showers. Medications need steady 59°F-77°F (15°C-25°C). Bathrooms regularly blast past that.
Humidity is the main enemy of medication stability. Tablets absorb water leading to hydrolysis, capsules become brittle or sticky, and powders clump together. A study in Circulation found that improper storage of beta-blockers resulted in inconsistent blood pressure control in 30.2% of monitored patients. That's a direct link between bathroom storage and life-threatening health risks.
Medicines That Fail in the Bathroom
Insulin is a protein-based medication that breaks down fast above 86°F (30°C). Even a few hours in a hot bathroom can ruin it, causing dangerous blood sugar spikes. Nitroglycerin tablets-used for heart attacks-lose potency rapidly in humid air. Birth control pills? FDA stability testing shows humidity can reduce contraceptive effectiveness by up to 35%. And antibiotics? If they degrade, infections may not clear up, contributing to antibiotic resistance. The World Health Organization warns this makes infections harder to treat globally.
Baystate Health's research shows most medications need strict temperature control. Bathrooms regularly spike 20-30°F during showers. A single hot shower can push a medicine cabinet above 90°F. Insulin vials left in that heat become cloudy or clumpy. That's not just inconvenient-it's dangerous. People with diabetes could get dangerously high blood sugar if their insulin fails.

Safety Risks Beyond Effectiveness
Storing opioids in bathroom cabinets? That's a danger sign. CDC data shows 70% of misused prescription opioids originate from home medicine cabinets. And kids? A NIH-funded study found 63% of households with minors keep high-risk meds within reach. The American Academy of Pediatrics says all medications should be stored in locked cabinets out of children's reach. Same goes for pets-70% of pet poisonings involve household meds, according to the ASPCA.
Controlled substances like oxycodone or fentanyl patches stored in unsecured bathroom cabinets create easy access for curious teens or burglars. This isn't just a "what if" scenario-it happens daily. In 2022, emergency rooms treated over 100,000 children for accidental medication poisoning, with bathrooms being the top source.
Where to Store Medicines Properly
Keep meds in a cool, dry place. A locked bedroom drawer works best. Avoid cars or windowsills too. For refrigerated meds like insulin, use a dedicated fridge-not the kitchen unit that opens often. Kaiser Permanente's medication management protocol specifies storing in "a cool, dry place" away from heat sources, sunlight, and moisture. ECRI Institute guidelines say medications requiring refrigeration must be kept between 36°F-46°F (2°C-8°C) in pharmaceutical refrigerators.
Think about your bedroom. Interior closets or dressers away from windows stay stable. Temperature there rarely changes more than 2-3°F daily. Compare that to bathrooms, which swing 15-20°F. A study in the Journal of Pharmacy Practice found properly stored medications maintain 98.7% potency after six months. Bathroom-stored meds? Just 72.3% left. That's a massive drop in effectiveness.

Safe Disposal: Protect People and the Planet
Don't flush old pills. The EPA says that pollutes waterways. Instead, use pharmacy take-back programs or mix meds with coffee grounds in a sealed bag before trashing. The NIH estimates $98 million worth of unused meds sit in US homes-proper disposal protects both people and the planet.
Pharmacy take-back programs are available at most pharmacies or police stations. They safely destroy medications without environmental harm. If none are nearby, the FDA recommends mixing pills with unappealing stuff like cat litter or coffee grounds in a sealed container before tossing. This prevents accidental ingestion and keeps drugs out of water systems.
Frequently Asked Questions
Can I store meds in a kitchen cabinet?
Kitchen cabinets are usually okay if they're away from the stove or sink. But avoid places near heat sources like the oven or dishwasher. A cool, dark interior cabinet is better than a bathroom. Always check the specific storage instructions on your medication label.
What should I do with expired medications?
Never flush them down the toilet. Use pharmacy take-back programs or mix them with coffee grounds or cat litter in a sealed bag before throwing in the trash. Some communities have drug disposal events-check local health department websites. Proper disposal prevents environmental contamination and accidental poisoning.
How often should I check my medicine cabinet?
Clear out expired or unused meds every three months. Great Ormond Street Hospital in London advises this because "many medicines 'go off' after a while" in suboptimal conditions. Check expiration dates regularly-some meds like nitroglycerin degrade in months, not years.
Are there special storage rules for insulin?
Unopened insulin vials need refrigeration between 36°F-46°F (2°C-8°C). Once opened, most can stay at room temperature for 28-30 days. But never leave them in a hot car or bathroom. If insulin looks cloudy or has particles, toss it immediately. Always follow the specific instructions on your bottle.
Why do some meds have humidity indicators?
Many prescription bottles now include humidity-indicating desiccant packets. These change color if moisture gets in. About 58% of prescription bottles have these now. If you see a color change, your meds might be degraded. Replace them immediately. This tech helps catch storage issues before they cause health problems.



Comments (9)