Drug Interaction: What You Need to Know About Medication Risks
When you take more than one medication, your body doesn’t always treat them like separate guests—it sees them as guests who might fight over the same room. This is what we call a drug interaction, a change in how a drug works when combined with another drug, food, supplement, or medical condition. Also known as medication interaction, it’s not just a technical term—it’s a real risk that can turn a safe treatment into a dangerous one. You might be taking warfarin for blood thinning, sertraline for depression, or even vitamin C for your skin, but none of these exist in a vacuum. Each one can react with others in ways your doctor might not immediately catch if you don’t speak up.
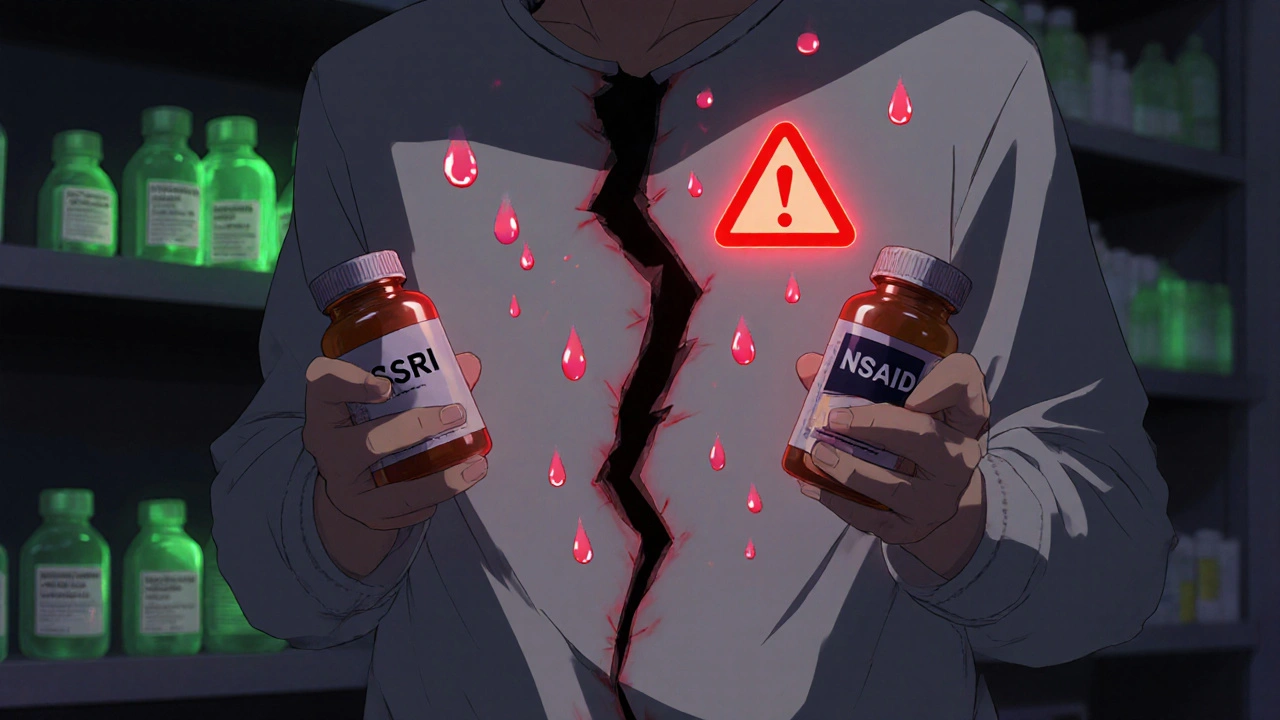
Some drug interactions, happen when one drug changes how your body absorbs, breaks down, or gets rid of another. Also known as pharmacokinetic interaction, this is why you can’t mix sertraline with certain NSAIDs or alcohol—it increases bleeding risk or triggers serotonin syndrome. Other types, called pharmacodynamic interactions, occur when two drugs have similar or opposite effects on your body. Also known as drug effect interaction, this is what makes combining warfarin with vitamin K-rich foods or certain supplements like vinpocetine risky. Even something as simple as calcium carbonate in antacids can block absorption of other pills if taken at the same time.
People often don’t realize how common these clashes are. One in five adults takes five or more medications. That’s not just a number—it’s a ticking clock if no one’s checking for overlaps. Your doctor might know about your prescription, but do they know you’re taking Emergen-C every morning or that you’ve been using Tugain for hair loss while on a beta-blocker? These aren’t side notes—they’re critical data points. And if you’re switching from one drug to another, like moving from Isordil to a different heart medication, or swapping Flomax for another BPH treatment, you’re not just changing brands—you’re changing how your body responds to everything else.
There’s no magic checklist for every interaction, but there are clear patterns. Blood thinners like warfarin are notorious for clashing with supplements, antibiotics, and even grapefruit. Antidepressants like vilazodone and sertraline can cause serious reactions when mixed with other mood drugs or painkillers. And don’t assume natural means safe—vinpocetine, vitamin C, and diacerein all have hidden risks when layered with prescription meds. The real danger isn’t the drug itself—it’s the silence around it. Most people don’t report their supplements to their doctor. They think it’s not important. But it is.
Below, you’ll find real-world examples from people who’ve been there: women switching from warfarin to heparin during pregnancy, patients spotting serotonin syndrome after mixing sertraline with ibuprofen, and others learning how to safely buy generic versions without risking dangerous combos. These aren’t theoretical scenarios—they’re lived experiences. What you’ll find here isn’t just a list of warnings. It’s a practical guide to asking the right questions, recognizing the signs, and protecting yourself before it’s too late.